Articles
Leonel dos Santos Silva 1
Bruna Eloise Lenhani 2
Dabna Hellen Tomim 3
Paulo Ricardo Bittencourt Guimarães 4
Luciana Puchalski Kalinke 5
1 ![]() 0000-0002-8359-5622. Universidade
Federal do Paraná (UFPR), Brazil. leonel.silva@hc.ufpr.br
0000-0002-8359-5622. Universidade
Federal do Paraná (UFPR), Brazil. leonel.silva@hc.ufpr.br
2 ![]() 0000-0002-6009-3400. Hospital
Erasto Gaertner, Brazil. blenhani@erastogaertner.com.br
0000-0002-6009-3400. Hospital
Erasto Gaertner, Brazil. blenhani@erastogaertner.com.br
3 ![]() 0000-0003-3199-0740 Universidade Federal do Paraná (UFPR), Brazil. dabnatomim@ufpr.br
0000-0003-3199-0740 Universidade Federal do Paraná (UFPR), Brazil. dabnatomim@ufpr.br
4 ![]() 0000-0002-9852-6777.Universidade
Federal do Paraná (UFPR), Brazil. prbg@ufpr.br
0000-0002-9852-6777.Universidade
Federal do Paraná (UFPR), Brazil. prbg@ufpr.br
5 ![]() 0000-0003-4868-8193. Universidade
Federal do Paraná (UFPR), Brazil. lucianakalinke@ufpr.br
0000-0003-4868-8193. Universidade
Federal do Paraná (UFPR), Brazil. lucianakalinke@ufpr.br
Received: 23/02/2019
Sent to peers: 12/03/2019
Approved by peers: 16/04/2019
Accepted: 09/05/2019
10.5294/aqui.2019.19.3.7
Theme: Chronic care
Contribution to the discipline: Advanced cancer results in multidimensional alterations of the quality of life. In this scenario, identifying those changes is a global health priority, given that knowing to intervene in the plurality of sufferings experienced by patients and their families is one of the principles of the palliative intention. For nursing, promoting the process based on validated and feasible instruments, and indicating the common alterations in the therapeutics and in palliative care, will aid in holistic care and can favor the quality of life. As for teaching, it contributes to the training of professionals who are aware of the needs of patients with advanced cancer, supported by a philosophy of palliative care.
To reference this article / Para citar este artigo / Para citar este artículo : Silva LdS, Lenhani BE, Tomim DH, Bittencourt PR, Kalinke LP. Quality of Life of Patients with Advanced Cancer in Palliative Therapy and in Palliative Care. Aquichan 2019; 19(3): e1937. DOI: https://doi.org/10.5294/aqui.2019.19.3.7
|
Abstract Objective: To
assess the quality of life of patients with advanced cancer in palliative
therapy and in palliative care. Keywords (source DeCS): Quality of life; advanced cancer; neoplasm; cancer pain; palliative care; hospice care; oncology nursing. |
Resumen Objetivo: evaluar la calidad de vida de pacientes con cáncer
avanzado en tratamiento paliativo y cuidado paliativo. Palabras clave (fuente DeCS): Calidad de vida; cáncer avanzado; neoplasias; dolor en cáncer; cuidados paliativos; cuidados paliativos al final de la vida; enfermería oncológica. |
Resumo Objetivo: avaliar a qualidade de vida de pacientes com câncer
avançado em terapêutica paliativa e em cuidado paliativo. Palavras-chave (fonte: DeCS): Qualidade de vida; câncer avançado; neoplasias; dor do câncer; cuidados paliativos; cuidados paliativos na terminalidade da vida; enfermagem oncológica. |
Introduction
Approximately 90 % of deaths of patients with cancer are related to the advanced stage of the disease, which are due to the late diagnosis and treatment. Advanced cancer (AC) becomes progressive and incurable, resulting in diminished functional capacity, increased burden of symptoms, and significantly compromises the quality of life (QoL) (1, 2).
For patients with AC, the treatment offered is palliative therapy (PT) and/or palliative care (PC). The PT aims to minimize the symptoms, control the side effects, and improve the QoL, but without prolonging the survival. It indicates the use of systemic treatments (chemotherapy, hormone therapy, and immunotherapy), radiation, and surgery (3).
The conceptions of PC are founded on a philosophy of care that promotes the QoL of patients and their relatives in confronting diseases that threaten the continuity of life, through prevention and relief from suffering (4). It has to do with comprehensive care focused on relief from suffering and requires the identification of pain, its evaluation, and treatment, besides other problems of physical, psychosocial, and spiritual nature to provide better QoL (5).
The concept of QoL is a central element and one of the objectives of PC: Professionals, patients, their families, and the community must have some shared comprehension of this philosophy of care (5). QoL is understood as “the perception of individuals of their position in life, within the context of culture and systems of values in which they live and in relation to their objectives, expectations, standards and concerns” (6). It is a complex construct that considers subjective, multidisciplinary, and bipolar aspects (7), which, with the aid of valid instruments, it is possible to identify and measure.
Even when referring to diseases beyond the possibilities of cure, patients and professionals must decide for therapeutic measures aimed at maximizing QoL (7). The differences between PT and PC are frequently misunderstood by patients and professionals due to faults in communication, acceptance, and in psycho-cultural aspects related with AC (8).
This research is justified by the need to identify the altered domains as an evaluation strategy to guide care practices in maintaining the functional capacity and in controlling symptoms in the palliative modalities in oncology, as well as contributing to the formulation of public health policies focused on the theme. In this sense, this study sought to assess the quality of life of patients with AC in PT and PC.
Materials and methods
This was a quantitative, observational, cross-sectional, and analytical research. It was conducted with hospitalized patients or in outpatient care, cared by multi-professional teams specialized in oncology and PC from a public hospital located in the southern region of Brazil.
The inclusion criteria used were: Patients over 18 years of age, with AC, aware of their mode of treatment and who had functional capacity according to the Eastern Cooperative Oncology Group (ECOG) scale of 0, 1, 2, 3, or 4 (9). The study also considered the registry in the medical record of the mode of treatment.
The ECOG is a scale that describes the functioning level of patients in terms of their capacity to care for themselves, daily activity, physical disability; it has a classification from 0 to 5. At 0, the patient is totally active, capable of conducting all pre-disease performance without restriction; 5 (five) is when the patient is dead (9).
The study excluded patients who did not communicate verbally and those who had already participated in the study at another moment during hospitalization or in the outpatient service, given that outpatients were referred for hospitalization and subsequently assigned to outpatient follow-up when they presented satisfactory evolution.
The sample was non-probabilistic, collected from January to June 2018, with a population of 126 patients: 107 in PT, and 19 in exclusive PC. This type of sampling was chosen due to the unavailability of a precise number of patients attended in previous years because the insertion of the PC staff is relatively new in the institution, which made it impossible to perform the sample calculation.
The data collection was carried out in the care units, in the waiting room and/or in outpatient procedures, or in nursing during hospitalization. After confirming the inclusion criteria and the authorization to participate in the research, patients answered the questionnaire or it was read by the researcher, without giving explanations and/or expressions, to avoid interfering in the responses and ensure impartiality. Said strategy enabled participants with limitations of reduced functional capacity imposed by the disease and by the treatments to be included in the study.
During the data collection, four distinct instruments were applied: The Questionnaire of Sociodemographic and Clinical Variables, the Quality of Life Questionnaire Care 15 Palliative (EORTC QLQ-C15-PAL), the Functional Assessment of Chronic Illness Therapy-Palliative Care 14 (FACIT-Pal-14), and the Edmonton Symptom Assessment System (ESAS).
The EORTC QLQ-C15-PAL instrument, developed by the European Organization for Research and Treatment of Cancer (EORTC), was translated and validated in Brazil. It is composed of 15 questions in the Likert scale format, scores range from 0 to 100 for physical function, emotional, symptoms (higher score in the functional scales indicate better QoL, contrary to that observed in the scale of symptoms) and overall QoL (from 1 to 7 points, the higher the score, the better the QoL) (10).
The FACIT-Pal-14, developed by the American group Functional Assessment of Chronic Illness Therapy (FACIT), has 14 items in Likert scale format, with statements about the last seven days, with respective scores for physical and functional wellbeing (0-16 points), social/family wellbeing (0-4), emotional wellbeing (0-8), and additional concerns (0-20), which results in the total score (0-56). The higher score is indicative of better perception of QoL (11). To make the comparison feasible, FACIT-Pal-14 scores were transported to a 100-point scale.
The ESAS was used to evaluate the symptoms: Pain, tiredness, nausea, depression, anxiety, drowsiness, appetite, wellbeing, shortness of breath, and any specific symptom (12). It is a visual numerical scale with 11 points (0 to 10) and, the higher the score, worse is the intensity of the symptoms; classified as mild (1-3), moderate (4-6), or intense (≥ 7) (13).
The use of the EORTC QLQ-C15-PAL, FACIT-Pal-14, and ESAS questionnaires is justified by the lack of a psychometric tool that evaluates the altered domains in palliative patients (14).
All the data gathered were tabulated in Microsoft Excel® 2016, analyzed by descriptive statistics expressed in relative frequency, absolute (%), mean, minimum, maximum, and standard deviation. The correlations were evaluated by Spearman’s non-parametric coefficient, given that the data analyzed do not suggest a normal distribution. All effects were considered significant and the relationships associated with values of p < 0.05. The QoL scores considered were poor (0-25), regular (26-50), good (51-75), and optimal (76-100).
This research was approved by the Institution’s Ethics and Research Committee with code # 2.461.307.
Results
The sociodemographic and clinical characterization of the sample in Table 1 shows that the mean age of the PT/PC groups was 58.3/62.6 years, respectively; female sex was prevalent by 61.68 % (n = 66) in the PT group and 57.89 % (n = 11) in the PC; the marital status of married or in common law was 58.88 % (n = 63) in the PT and 52.63 % (n = 10) in the PC. Regarding the diagnosis, 28.97 % (n = 31) in the PT group and 15.79 % (n = 3) in the PC had breast cancer; the functional capacity was classified at 75.7 % (n = 81) (ECOG 1 and 2) for the PT group and 89.47 % (n = 17) (ECOG 2 and 3) for the PC.
Table 1. Sociodemographic and clinical characteristics of patients with AC in PT and in PC

Source: Own elaboration.
Regarding the EORTC QLQ-C15-PAL questionnaire, it was possible to observe that, in the assessment of overall health status, patients in PT had better QoL score (71.54), compared with the PC group (59.65), but without significance between the groups. When evaluating the physical and emotional function, PT presents scores of 17.95 and 28.83, and the PC group of 53.67 and 43.87, respectively; this represents better QoL in these domains for patients in PC, with significance in the physical function (p = 0.000). In relation to the scale of symptoms, unsatisfactory QoL in the PT group with greater suffering for nausea/vomit and fatigue, with scores of 73.84 and 63.45; and the scores for the respective symptoms in the PC group were 38.58 and 48.25, which indicates better QoL.
With respect to the FACIT-Pal-14 instrument, the means of the total score and of the domains indicated better QoL in the PT group, compared with the PC. Except for the item “I am concerned that my state will get worse” from the scale of emotional wellbeing, 34.35/55.26 (p = 0.022).
The evaluation of symptoms with the ESAS questionnaire indicated lower suffering in the PT group compared to patients in PC, both in the total score 27.99/39.3 (p = 0.014) and in the symptoms of greater intensity, like drowsiness 3.22/5.68 (p = 0.005), appetite 3.61/5.95 (p = 0.004), wellbeing 3.74/5.58 (p = 0.014).
The scores of General Quality of Life (GQoL) evaluated with the EORTC QLQ- C15-PAL, described in Table 2, when correlated with the FACIT-Pal-14 domains and the ESAS total score, in the PT, showed a significant correlation, except for the additional concerns, which indicates that this domain was not significant in the QoL of this group. In PC, the correlation occurred in the functional domains (p = 0.008 and p = 0.046), social/family (p = 0.001), and emotional for the worsening state (p = 0.008); the correlation shows the significance of these domains in the QoL of patients in the study.
Table 2. Spearman correlation between GQoL (EORTC QLQ-C15-PAL) and domains (FACIT-Pal-14) and of ESAS of patients with AC in PT and in PC
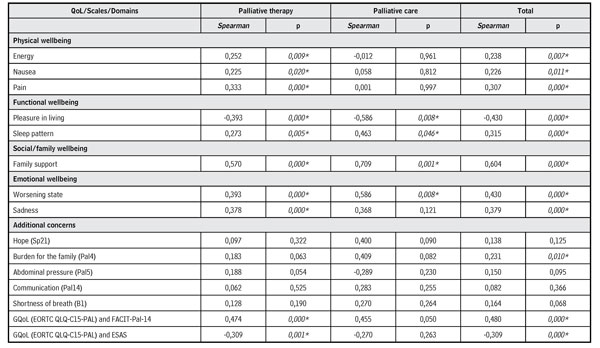
Source: Own elaboration.
When evaluating the relationship between the FACIT-Pal-14 scores and the ESAS total score (Table 3), it was observed that the physical and emotional function was better in patients with decreased multidimensionality of symptoms; similar results in both groups of patients.
Table 3. Ratio of scores of the FACIT-Pal-14 domains with the ESAS total score of patients with AC in PT and in PC
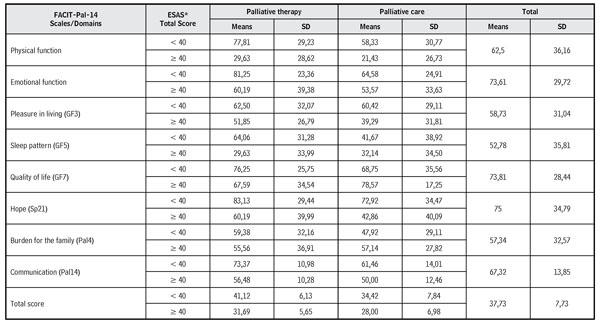
*ESAS Total score: < 40, mild symptoms and ≥
40, moderate and intense symptoms.
Source: Own elaboration.
In the correlation (Table 4) of the total score of symptoms of the ESAS scale with the total score with the domains of the FACIT-Pal-14, significance was observed among the variables for PT in the domains of physical, functional, social/family, emotional wellbeing, and additional concerns. In the PC, some items were correlated, like: Functional wellbeing (pleasure in living), emotional wellbeing (concern with worsening of their status), and additional concerns (burden for the family). There is also a significant correlation between the total score of symptoms of the ESAS and the QoL of the FACIT-Pal-14 in both groups, which indicates the interference of burden and of the intensity of symptoms in QoL.
Table 4. Spearman correlation between total score of symptoms of ESAS and domains (FACIT-Pal-14) of patients with AC in PT and in PC
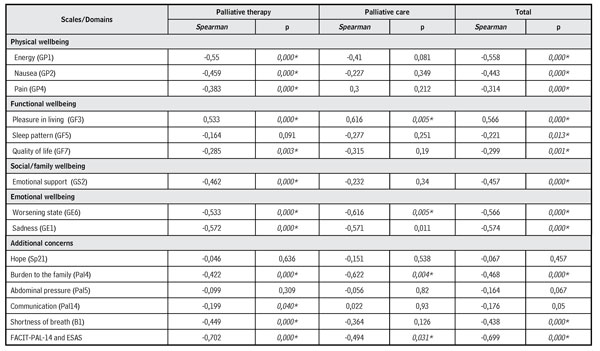
Source: Own elaboration.
Discussion
Advanced cancer brings to the lives of patients and their relatives changes in multidimensional aspects that affect the QoL. Hence, it becomes necessary to consider the interference of sociodemographic characteristics in research and in care practices. The perception of QoL can be altered by sex, age, schooling, daily life activities, education, and by the number of children; it is up to the nurses to know said predictors that impact QoL to propose a care plan (15, 16).
The prevalence of the female sex in the research is not corroborated with the 2018 cancer estimate in Brazil (17), nor with the study conducted in Taiwan with patients in PT and PC in which the male sex was prevalent in both groups, 73.7 % and 61.6 %, respectively (18). A fact possibly related with the geographic distribution, population density, risk factors, and with public health policies. For marital status, similarity exists with the conducted in São Paulo, Brazil, in which 61.5 % had a permanent mate (19). A Korean study evidenced that married women with AC had less symptoms, consequently, better QoL than women who were single (20).
An impact factor for the choice of treatment is the QoL score is the functional capacity. In this study, patients in PT had better ECOG, while those in PC were more clinically debilitated. In practice, it is perceived that the greater decline in functional capacity, greater is the probability of indication of exclusive PC to the patient. A retrospective study in São Paulo, Brazil, conducted with 301 patients in PT classified with ECOG greater too r equal to 2, evidenced the need for caution in the indication of palliative chemotherapy, given that they did not have benefits in overall survival and in GQoL (21).
The GQoL in the present research had a better total score in the PT group in relation to the PC group. This data agreed with the study carried out in the southeastern region of Brazil, which evidenced that patients in PT (median 66,7) had better GQoL than those in PC (median 50) (p > 0.01). In the translation of the QLQ-C15-PAL with patients in PT conducted in China, the mean score was 46.63, and significant variations (p = 0.000), based on the functional capacity, means of 50.81 (ECOG 0-2) and 37.66 (ECOG 3-4) (22). These data reinforce that a worse functional performance results in diminished GQoL, physical and emotional function, and increases suffering through the intensity of symptoms.
However, in AC, the benefits of PT in survival and in QoL can be modest, compared with the high cost and with the toxicity, which can be minimized with the early insertion of PC. Psychometric measurements can identify early the lack of control of symptoms, as well as other clinical outcomes that diminish the QoL (23). Thus, nurses must act constantly to identify altered multidimensional aspects that decrease the QoL and participate actively on the offer of PC, especially in patients who endure AC.
The GQoL of patients in exclusive PC, who participated in this research, was classified as regular. Better results (68.45) were found in the study with 29 hospitalized patients in the central-eastern region of Brazil (24). But, in the psychometric validation of the EORTC QLQ-C15-PAL, conducted in Turkey, with 150 hospitalized patients and with limitation of the functional capacity (ECOG ≥ 3), the score was 30 in GQoL, associated to worse physical and emotional function (p = 0.026) (25).
Such divergence is probably related with AC, a factor that impacts upon the QoL of individuals, given the progression of the disease or the treatment recommended (26). The evolution of modifying clinical conditions is directly associated with decreased functional capacity and QoL, which require early identification and intervention.
A study conducted in the southeast region of Brazil, with the objective of evaluating the QoL of nine patients inserted in the exclusive PC and hospitalized in an oncology unit, evidenced a total score of 84/184, which demonstrates regular QoL. The authors related the score to the lack of a service and to the incipient quantitative of human resources with palliative training in the research institution (27).
When comparing the study by Figueiredo, Souza, Coelho and Souza (27) with patients in PC from the present research, a similar total QoL score is verified; in addition, it is observed that the action time of the palliative team (physicians and nurses specialized in the action area) in the institution is relatively new and gradually evolves in the integration with the oncology staff.
In line with CP principles, integrated and interdisciplinary actions that promote QoL can positively impact the course of the disease, without seeking to anticipate or postpone the process of dying (4). When confronted with the data of the present study, management of patients in palliative intent is evident in unsatisfactory QoL conditions; a continuing need is highlighted to expand the range of institutional services and professional actions in line with this philosophy of care, anchored in better QoL.
Regarding the physical and emotional domains with the EORTC QLQ-C15-PAL, the PT group had worse scores when compared with the group of patients in PC, given that these are the functions with greatest impact on the treatment (28). In PT, variations of the physical function are related with the functional capacity (29), while in PC, the scores were better and diverged from expectations because they had greater limitations and predominantly because they were hospitalized (25).
In the assessment of physical and functional wellbeing measured with the FACIT- Pal-14, better scores were identified in patients in PT compared with the PC group. Early insertion of PC results in better QoL, (30); the altered scores need to be identified and controlled with interventions by Nursing aimed at the capacities and limitations of patients and their relatives (27). Encouraging positive coping, minimal development of labor/distractive activities, and awareness of limitations can contribute to improving QoL (31).
The EORTC QLQ-C15-PAL instrument pointed to an unsatisfactory QoL in both groups for the emotional function. The decrease in the domain that results in worse QoL is associated to functional capacity (25, 29). This domain presents a complex construct by involving feelings and affections, related to adequate psychosocial support provided by family and staff. It is relevant to consider the interference and adequate management of other symptoms that affect the patient’s communication, dyspnea, for example (24).
In the evaluation with the FACIT-Pal-14 instrument, emotional wellbeing presented significance in the PC group in relation with PT; the decrease in this domain can also be associated to the progression of health conditions and uncontrolled symptoms (fatigue, insomnia, feeding difficulties, gastrointestinal disorders, appearance, and pain) (27).
With respect to the emotional dimension, professionals can launch some strategies to improve QoL; encouraging patients to visualize the positive aspects in confronting the disease, encouraging the fight against negative emotions and stimulating the presence of loved ones. Improved emotional wellbeing is related with social wellbeing; professionals can promote these strategies with support from other people (31).
In relation to social/family wellbeing, QoL in both groups showed satisfactory similarities in the PT and PC groups; said information reinforces the importance of support perceived in social interactions (relatives, friends, and health staff). Social wellbeing comprises the perception of support, associated to emotional, informational, and care support, as well as to being accompanied; said measures result in improved QoL and physical and psychological benefits (32). Professionals caring for this public need to refine communication and perception skills to identify said changes, seeking better support for patients.
Within this context, one of the priority goals of PC is the relief from emotional suffering and improved wellbeing for patients and caretakers (4). Given the importance of adequate evaluation to keep emotional suffering from being underestimated, when it is identified, it needs specific therapeutic interventions with qualified professionals (33).
The scale of symptoms, assessed with the EORTC QLQ-C15-PAL instrument, shows that higher score indicates worse QoL. In the PT group, nausea/vomit and fatigue, the later was the most intense symptom in the evaluation with said instrument and with the ESAS, possibly associated to the active systemic treatment. In PC, symptoms differ, by pointing to pain and nausea/vomit as responsible for the decline in QoL, and worse intensity for loss of appetite in the ESAS evaluation. Among the unpleasant symptoms, the perception of nausea/vomit may result in physiological complications, and fatigue is frequently present with management difficulties; consequently, both deteriorate QoL (2, 34).
In the assessment of symptoms with the ESAS, results from the national (35) and international (36, 37) literature differ regarding the symptoms and the intensity in the PT and PC groups in this research; such divergences are related to type of cancer, presence of metastases, treatment used, adequate management of symptoms, among others. Evaluating the symptomatic burden and identifying the decrease in functional capacity are indirect ways of measuring QoL.
Controlling the unpleasant symptoms is at the heart of the philosophical framework of PC; such need is a priority in patients and extended to the family members (4). This strategy is corroborated by specialists in AC, who indicate that the assessment and management of symptoms must be conducted periodically and guided by valid instruments, as well as the reference to specialized services when uncontrolled (38). However, this research shows that, even in specialized services, patients have not fully controlled symptoms, a fact that points out discrepancies between clinical practice and PC principles.
Regarding the subjective and multidimensional dimension of the individual perception of QoL, a diversity of factors interferes in its measurement and, among those previously cited, the functional capacity, uncontrolled symptoms, and treatments proposed can interfere positively or negatively in the evaluation. Such evidence permits reflecting on the periodic need for evaluation, given that patients in PT undergo some active treatment and, in PC, the goal is the control of symptoms; however, the premise of both is to maximize QoL.
Given the importance of the theme, the measurement of symptomatic load and QoL are essential to guide care needs, assess the effectiveness of the implementations, and indicate the best evidences to be proposed to patients with AC. However, in Brazil, the scarcity of comprehensive research and data on QoL in palliative patients hinders confrontation with the cultural context and with health systems (26).
Conclusion
In the evaluation with the EORTC QLQ-C15-PAL instrument, the overall QoL was indicated as good in the PT group and regular in the PC. In relation to physical and emotional function and to the scale of symptoms, the scores indicate better QoL in the PC group. The FACIT-Pal-14 instrument shows better QoL in the PT group, with higher means in total score, diverse items from the scale of physical, functional, social/family, and palliative wellbeing.
In the correlation of the GQoL score of the EORTC QLQ-C15-PAL with the FACIT-Pal-14 domains and with the ESAS total score, the PT group only had significance in the domains of physical, functional, and social/family wellbeing. The relation between the FACIT-Pal-14 scores with the total ESAS score corroborates that the physical and emotional function is better in the PT group for patients with mild symptoms.
With respect to the ESAS evaluation, the PT group presents mild symptoms; while the PC group shows higher intensity and significance (somnolence, appetite, wellbeing, and total score), possibly related with decreased functional capacity and late accompaniment from palliative professionals, which need to be periodically evaluated and controlled to improve the QoL, the principal objective of said philosophy of care. In the correlation of the ESAS with the FACIT-Pal-14, the domains are significant in the PT group.
Among the contributions of the study, we can highlight the existence of differences in the burden of symptoms and in the QoL of patients with AC included in PT and PC, which need to be evaluated for the implementation in the process of care by health professionals and, consequently, adopt interventions in the clinical practice to provide improved QoL, based on the principles of PC.
Among the limitations of the study, we can point to the small size of the sample of patients in the PC group and to the fact of having been conducted in a single center. Future studies must be carried out to elucidate the plurality of assessments and palliative interventions, principally with the use of FACIT-Pal- 14, given the scarcity of research with this instrument.
Conflict of interest: None declared.
References
1. Weinberg RA. The biology of cancer. 2nd ed. New York: Garland Science, 2014. 728 p.
2. Dong ST, Costa DSJ, Butow PN, Lovell MR, Agar M, Velikova G et al. Symptom clusters in advanced cancer patients: An empirical comparison of statistical methods and the impact on quality of life. J Pain Symptom Manage. 2016; 51(1):88-98. DOI: 10.1016/j.jpainsymman.2015.07.013
3. Cancer Research. Palliative treatment [Internet]. 2018 [cited 2018 sep 21]. Disponível em: https://www.cancerresearchuk.org/about-cancer/cancer-in-general/treatment/palliative
4. World Health Organization (WHO). Global atlas of palliative care at the end of life [Internet]. 2014 [acesso em 21 set. 2018] 111 p. Disponível em: http://www.who.int/nmh/Global_Atlas_of_Palliative_Care.pdf
5. Knaul FM, Farmer PE, Krakauer EL, De Lima L, Bhadelia A, Jiang Kwete X et al. Alleviating the access abyss in palliative care and pain relief — an imperative of universal health coverage: The Lancet Commission report. Lancet. 2018; 391(10128):1391-454. DOI: 10.1016/S0140-6736(17)32513-8
6. Ghandourh WA. Palliative care in cancer: managing patients’ expectations. J Med Radiat Sci. 2016; 63(4):242-57. DOI: 10.1002/jmrs.188
7. World Health Organization (WHO). WHOQOL: measuring quality of life. Psychol Med [Internet]. 1998 [citado em 12 nov. 2018]; 28(3):551-8. Disponível em: http://www.who.int/mental_health/media/68.pdf
8. Romero M, Vivas-Consuelo D, Alvis-Guzman N. Is Health Related Quality of Life (HRQoL) a valid indicator for health systems evaluation? Springerplus. 2013; 2(1):664. DOI: 10.1186/2193-1801-2-664
9. Oken M, Creech R, Tormey D, Horton J, Davis T, McFadden E et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982; 5(6):649-56. Disponível em: https://journals.lww.com/amjclinicaloncology/Abstract/1982/12000/Toxicity_and_response_criteria_of_the_Eastern.14.aspx
10. Groenvold M, Petersen MA, Aaronson NK, Arraras JI, Blazeby JM, Bottomley A et al. The development of the EORTC QLQ-C15-PAL: A shortened questionnaire for cancer patients in palliative care. Eur J Cancer. 2006; 42(1):55-64. DOI: 10.1016/j.ejca.2005.06.022
11. Zeng L, Bedard G, Cella D, Thavarajah N, Chen E, Zhang L et al. Preliminary results of the generation of a shortened quality-of-life assessment for patients with advanced cancer: the FACIT-Pal-14. J Palliat Med. 2013; 16(5):509-15. DOI: 10.1089/jpm.2012.0595
12. Bruera E, Kuehn N, Miller MJ, Selmser P, Macmillan K. The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care [Internet]. 1991 [acesso em 18 fev. 2019]; 7(2):6-9. Disponível em: https://psycnet.apa.org/record/1991-34179-001
13. McGee SF, Zhang T, Jonker H, Laurie SA, Goss G, Nicholas G et al. The Impact of Baseline Edmonton Symptom Assessment Scale Scores on Treatment and Survival in Patients with Advanced Non-small-cell Lung Cancer. Clin Lung Cancer. 2017; 19(1):91-9. DOI: 10.1016/j.cllc.2017.05.018
14. McCaffrey N, Bradley S, Ratcliffe J, Currow DC. What Aspects of Quality of Life Are Important from Palliative Care Patients? Perspectives? A Systematic Review of Qualitative Research. J Pain Symptom Manage. 2016; 52(2):318-28. DOI: 10.1016/j.jpainsymman.2016.02.012
15. West C, Paul SM, Dunn L, Dhruva A, Merriman J, Miaskowski C. Gender Differences in Predictors of Quality of Life at the Initiation of Radiation Therapy. Oncol Nurs Forum. 2015; 42(5):507-16. DOI: 10.1188/15.ONF.507-516
16. Trinquinato I, da Silva RM, Benavente SBT, Antonietti CC, Calache ALSC. Gender differences in the perception of quality of life of patients with colorectal cancer. Investig y Educ en Enferm. 2017; 35(3):320-9. DOI: 10.17533/udea.iee.v35n3a08
17. Instituto Nacional do Câncer (Brasil). Estimativa 2018 — Incidência de câncer no Brasil. 2018 [acesso em 12 nov. 2018. 130 p. Disponível em: https://www.inca.gov.br/publicacoes/livros/estimativa-2018-incidencia-de-cancer-no-brasil
18. Wu CC; Hsu TW, Chang CM, Lee CH, Huang CY, Lee CC. Palliative Chemotherapy Affects Aggressiveness of End-of-Life Care. The Oncologist. 2016; 21(6):771-7. DOI: 10.1634/theoncologist.2015-0445
19. Matos TD de S, Meneguin S, Ferreira M de L da S, Miot HA. Qualidade de vida e coping religioso-espiritual em pacientes sob cuidados paliativos oncológicos. Rev Lat Am Enfermagem. 2017; 25: e2910. DOI: 10.1590/1518-8345.1857.2910
20. Han K, Kim SJ, Song H, Chun S, Ok C, Kim J et al. Associations between Quality of Life and Marital Status in Cancer Patients and Survivors. Asian Pacific Asian Pacific J of Cancer Prevent. 2014; 15(13):5287-91. DOI: 10.7314/APJCP.2014.15.13.5287
21. Caires-Lima R, Cayres K, Protásio B, Caires I, Andrade J, Rocha L et al. Palliative chemotherapy outcomes in patients with ECOG-PS higher than 1. The Open Access Cancer J from the European Inst of Oncol and the OECI. 2018; 12(831):1-9. DOI: 10.3332/ecancer.2018.831
22. Zhang L, Wang N, Zhang J, Liu J, Luo Z, Sun W et al. Cross-cultural verification of the EORTC QLQ-C15-PAL questionnaire in mainland China. Palliative Med. 2015; 30(4):401-8. DOI: 10.1177%2F0269216315593671
23. LEE, Richard T. Meropol NJM. Rethinking the Value of Palliative Chemotherapy [Internet]. 2016 [citado 21 de set de 2017]; 9-12. Disponível em: http://am.asco.org/daily-news/rethinking-valuepalliative-chemotherapy
24. Matos GDR, Pulschen AC. Qualidade de Vida de Pacientes Internados em uma Unidade de Cuidados Paliativos: um Estudo Transversal. Rev Bras Cancerol [Internet]. 2015 [cited 2018 nov 12];61(2):123–9. Disponível em: http://www1.inca.gov.br/rbc/n_61/v02/pdf/06-artigo-qualidade-de-vida-de-pacientes-internados-em-uma-unidade-de-cuidados-paliativos-um-estudo-transversal.pdf
25. Ozcelik H, Guzel Y, Sonmez E, Aksoy F, Uslu R. Reliability and validity of the Turkish version of the EORTC QLQ-C15-PAL for patients with advanced cancer. Palliat Support Care. 2016; 14(6):628-34. DOI: 10.1017/S1478951516000195
26. Freire MEM, Costa SF, Lima RAG, Sawada NO. Qualidade de vida relacionada à saúde de pacientes com câncer em cuidados paliativos. Texto Contexto Enferm. 2018; 27(2):1-13. DOI: 10.1590/0104-070720180005420016
27. Figueiredo JF, Souza VM, Coelho HV, Souza RS. Qualidade de vida de pacientes oncológicos em cuidados paliativos. Rev Enferm do Centro-Oeste Min. 2018; 8:e2638. DOI: 10.19175/recom.v8i0.2638
28. Bedard G, Zeng L, Zhang L, Lauzon N, Holden L, Tsao M et al. Minimal important differences in the EORTC QLQ-C15-PAL to determine meaningful change in palliative advanced cancer patients. Asia Pac J Clin Oncol. 2016; 12(1):e38–46. DOI: 10.1111/ajco.12069
29. Nunes NAH. The quality of life of Brazilian patients in palliative care: Validation of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 15 PAL (EORTC QLQ-C15-PAL). Support Care Cancer. 2014; 22(6):1595–600. DOI: 10.1007/s00520-014-2119-1
30. Bakitas MA, Dragnev KH, Bakitas MA, Tosteson TD, Li Z, Lyons KD et al. Early Versus Delayed Initiation of Concurrent Palliative Oncology Care: Patient Outcomes in the ENABLE III Randomized Controlled Trial. J Clin Oncol. 2015; 3(13):1438-45. DOI: 10.1200/JCO.2014.58.6362
31. Frazer MS, Mobley P. A mixed methods analysis of quality of life among late-life patients diagnosed with chronic illnesses. Health Qual Life Outcomes. 2017; 15:222. DOI: 10.1186/s12955-017-0797-3
32. Bradley N, Lloyd-Williams M, Dowrick C. Effectiveness of palliative care interventions offering social support to people with life-limiting illness — A systematic review. Eur J Cancer Care (Engl). 2018;27(3):1-12. DOI: 10.1111/ecc.12837
33. Smith H, Smith J, Smith A. An overview of nausea/vomiting in palliative medicine. Ann Palliat Med. 2012; 1(2):103-14. DOI: 10.3978/j.issn.2224-5820.2012.07.06
34. Paiva CE, Manfredini LL, Paiva BSR, Hui D, Bruera E. The Brazilian version of the Edmonton Symptom Assessment System (ESAS) is a feasible, valid and reliable instrument for the measurement of symptoms in advanced cancer patients. PLoS One. 2015; 10(7): e0132073. DOI: 10.1371/journal.pone.0132073
35. Yokomichi N, Morita T, Nitto A, Takahashi N, Miyamoto S, Nishie H et al. Validation of the Japanese Version of the Edmonton Symptom Assessment System-Revised. J Pain Symptom Manage. 2015; 50(5):718-23. DOI: 10.1016/j.jpainsymman.2015.05.014
36. Hannon B, Dyck M, Pope A, Swami N, Banerjee S. Modified Edmonton Symptom Assessment System Including Constipation and Sleep: Validation in Outpatients with Cancer. J Pain Symptom Manage. 2015; 49(5):945-52. DOI: 10.1016/j.jpainsymman.2014.10.013
37. Limonero JT, Lacasta Reverte MA, Gómez-Romero MJ, Gil-Moncayo F. The role of emotions in palliative care. Palliat Med Hosp Care Open J. 2018; 4(1): 7-9. DOI: 10.17140/PMHCOJ-4-127
38. Bickel KE, McNiff K, Buss MK, Kamal A, Lupu D, Abernethy AP et al. Defining High-Quality Palliative Care in Oncology Practice: An American Society of Clinical Oncology/American Academy of Hospice and Palliative Medicine Guidance Statement. J Oncol Pract, Alexandria. 2016;12(9): 828-38. DOI: 10.1200/JOP.2016.010686