Articles
Jessica Pamela Noack-Segovia 1
Antonio Manuel Sánchez-López 2
Inmaculada García-García 3
Raquel Rodríguez-Blanque 4
Ximena Alejandra León-Ríos 5
María José Aguilar-Cordero 6 .
1 ![]() 0000-0002-3463-9991. School of Nursing, Universidad de Santo Tomás, Chile. jnoack@santotomas.cl
0000-0002-3463-9991. School of Nursing, Universidad de Santo Tomás, Chile. jnoack@santotomas.cl
2 ![]() 0000-0001-5482-226X. CTS 367 Research Group, Junta de Andalucía, Spain. asanchez47@us.es
0000-0001-5482-226X. CTS 367 Research Group, Junta de Andalucía, Spain. asanchez47@us.es
3 ![]() 0000-0003-0500-7175. Faculty of Health Sciences, Universidad de
Granada, Spain. igarcia@ugr.es
0000-0003-0500-7175. Faculty of Health Sciences, Universidad de
Granada, Spain. igarcia@ugr.es
4 ![]() 0000-0003-2086-1222. Complejo Hospitalario
Universitario de Granada, Spain. rarobladoc@ugr.es
0000-0003-2086-1222. Complejo Hospitalario
Universitario de Granada, Spain. rarobladoc@ugr.es
5 ![]() 0000-0002-3494-331X. CTS 367 Research Group, Junta de Andalucía, Spain. ximenalr@correo.ugr.es
0000-0002-3494-331X. CTS 367 Research Group, Junta de Andalucía, Spain. ximenalr@correo.ugr.es
6 ![]() orcid.org/0000-0002-6268-0975 Faculty of Health Sciences, Universidad de Granada,
Spain. mariajoseaguilar@ugr.es
orcid.org/0000-0002-6268-0975 Faculty of Health Sciences, Universidad de Granada,
Spain. mariajoseaguilar@ugr.es
Received: 21/03/2019
Sent to peers: 22/04/2019
Approved by peers: 09/07/2019
Accepted: 17/07/2019
10.5294/aqui.2019.19.3.6
Theme: Promotion and prevention.
Contribution to the discipline: This research contributes to the care by expert health personnel in patients operated of bariatric surgery, given that it identifies common problems and proposes interventions that permit improvements in their health condition, like acquisition of healthy habits for patients and their families. Regaining weight in patients operated of bariatric surgery is quite frequent after two years, as indicated in the bibliography consulted, which is why patients and their families require support from a multidisciplinary team that lets them establish a relationship of trust.
To reference this article / Para citar este artículo / Para citar este artigo: Noack-Segovia JP, Sánchez-López AM, García-García I, Rodríguez-Blanque R, León-Ríos XA, Aguilar-Cordero MJ. Physical Exercise and Grip Strength in Patients Intervened through Bariatric Surgery. Aquichan 2019; 19(3): e1936. DOI: https://doi.org/10.5294/aqui.2019.19.3.6
|
Abstract Objective: This work sought
to evaluate a physical exercise program of moderate intensity in patients
operated of bariatric surgery and its influence on muscle strength. Keywords (source DeCS): Bariatric surgery; hand strength; exercise; exercise therapy; obesity; physical condition; obesity, morbid; physical activity; motor activity; body mass index. |
Resumen Objetivo: evaluar un programa de ejercicio físico de intensidad
moderada en pacientes operados de cirugía bariátrica y su influencia en la fuerza muscular. Palabras clave (fuente DeCS): Cirugía bariátrica; fuerza de la mano; ejercicio; terapia por ejercicio; obesidad; condición física; obesidad mórbida; actividad física; actividad motora; índice de masa corporal. |
Resumo Objetivo: avaliar um programa de exercício físico de intensidade moderada em pacientes submetidos à cirurgia bariátrica e sua influência na força muscular. Palavras-chave (fonte: DeCS): Cirurgia bariátrica; força da mão; exercício; terapia por exercício; obesidade; condição física; obesidade mórbida; atividade física; atividade motora; índice de massa corporal. |
Introduction
Morbid obesity has become a pandemic; it is not restricted to developed or developing countries, but encompasses all those with free-market economy systems (1). This problem, typical of recent decades, is a consequence of unhealthy habits of the population (2). Added to sedentary behavior, a result –in part– of the development of telecommunications, is the increased intake of foods with high contents of saturated fats. Currently, in the United States, one in every four children or adolescents suffers from obesity, and one in every three is at risk of acquiring it (3). Thus, one of every four overweight children, in the age range from 6 to 12 years, has glucose intolerance, and 60 % of them has at least one risk factor for cardiovascular disease (4). Childhood obesity is associated with a greater probability of premature death and disability in adulthood, and during adolescence it can reduce life expectancy from 5 to 20 years (5).
Bariatric surgery (BS) has meant a temporary solution against those cases in which, added to extreme weight, individuals develop pathologies associated with type II diabetes mellitus, hypertension, and locomotor problems, among others (6-9). After this intervention, patients experience rapid weight loss due to the notable decrease of fat-free mass (FFM) (10). Poor absorption of nutrients in the organism, added to inadequate intake of proteins produce a loss of muscle tissue and a considerable reduction of muscle strength (11).
The degree of caloric restriction, pre-operatory weight, advanced age, type II diabetes, exercise, and type of BS are known predictors of post-operatory loss of fat mass (FM) (10) (12). All the patients operated of BS have a strict follow up during the post-operatory to avoid recovering the weight lost and controlling possible alterations (11). What is sought is the loss of body fat, while preserving lean body mass (LBM), conformed by minerals, muscles, proteins, and bone (13); particularly, the body’s cell mass, which are part of the LBM. On average, LBM corresponds to 60 % - 90 % of the total body weight. Loss of LBM can be undesirable, given that this tissue is necessary for metabolic activity, regulation of body temperature, preservation of skeletal integrity, maintenance of hormone equilibrium, and perception of quality of life (14).
Avoiding muscle atrophy after BS is an essential part of post-operatory care and one of the reasons for using bioelectrical impedance analysis (BIA), a simple, rapid, and non-invasive technique that permits estimating total body water (TBW). Due to assumptions based on tissue hydration constants, FFM is obtained and, through derivation, FM, by the simple equation based on two components (FFM kg = total weight kg – FM kg). In the area of sports science, it is possible to measure TBW under different situations, during states of normal hydration, as during dehydration, as well evaluate body composition in diverse clinical and nutritional states related with physical activity and training (15).
Grip strength, which measures static muscle strength, has been used as predictor of functional capacity for various pathologies, given its easy application and low cost. This test has been used to predict mortality in patients with chronic obstructive pulmonary disease (COPD) and complications in patients on dialysis, as well as to assess malnutrition in hospitalized patients (16) (17).
Hypothesis
H0: A program of moderate physical activity does not produce significant changes in the intervention group.
H1: A program of moderate physical activity produces significant differences between the intervention group and the control group.
Objective
To evaluate a physical exercise program of moderate intensity in patients operated of BS and its influence on muscle strength.
Specific objectives
The following are the specific objectives of this study:
• To assess the muscle strength of patients operated of BS before and one month after the intervention.
• To evaluate the body composition of patients operated of BS before, one month after the intervention, and after a program of moderate exercise.
• To compare muscle strength and body composition in intervention groups and in control groups.
Methodology
This was a randomized clinical trial. Patients were divided into two groups: An intervention group (IG) and a control group (CG). Randomization was conducted via a random number generator on Excel. Then, baseline averages in both groups were compared through Student´s t test, obtaining values of p > 0.05, and tested the homogeneity of the baseline values of the samples. Inclusion criteria considered patients between 18 and 50 years of age, who had signed the informed consent, had no medical contraindications, acute myocardial infarction, heart failure, chronic pathologies with compromise of the general state, post-operatory complications, and who weighed less than 180 kilograms. The research was directed by a nurse, helped by a team comprising a physician, a nutritionist, and a physical therapist from the Lircay Clinic, where a BS program was carried out in which, annually, approximately 100 patients are operated. The clinic is privately run and it is located in the city of Talca, Chile.
A protocol was designed of educational interventions and moderate-intensity exercise. All the patients underwent an initial evaluation (anamnesis, anthropometric measurements, BIA, dynamometry). The IG participated in a moderate physical exercise program, one month after the surgery, and the CG received routine care, with monthly control by a physician and a nutritionist. The intervention lasted 24 weeks (18) (19) and was constituted by an education plan that included diet, physical exercise, and family support during the process. The nurse conducted controls once per month, together with the anthropometric measurements carried out by the nutritionist and the physical therapist. In addition, aerobic-type exercises and muscle strengthening work were planned, three times per week, and each session lasting one hour and a half. The participants were told they had to attend to 75 % of the training hours to be allowed to continue with the study.
Exercise protocol for the intervention group
The protocol described ahead began with an adaptation stage during two weeks, and then with a continuous stage, with the same routine, but in which the intensity and the repetitions increased gradually, under the supervision of a physical therapist.
The patients performed a walk at 54 % of their capacity and resistance frequency (FCdRes) on the treadmill (HP Cosmos®). The training intensity was modified to an intensity of 59 % of said frequency until completing the physical exercise program, with 30-min duration of aerobic training on the treadmill.
Muscular strengthening of biceps, triceps, deltoids, and pectorals was conducted progressively in intensity and number of repetitions, determined through the 1 Rmax evaluation. Training on the cycle ergometer (Monark®) was performed without load during 15 min. When the patient was not capable of conducting at least 10 min constantly, it was fractioned into two or three stages, intercalated with strengthening or elongation exercises. To finish the routine, upper and lower body elongation exercises were performed, plus respiratory exercises (inspiration, deep and diaphragmatic exhalation).
Measurements were taken 72 h after the last exercise session, in the same order and with the same physical therapy staff as in the baseline evaluation. All the subjects were instructed to refrain from any other type of physical activity during the intervention. The weight of patients was evaluated with a SECA-type scale; height was measured with a pedometer and body mass index (BMI) was calculated.
Ethical aspects
The project was approved by the Research Ethics Committee at Universidad Santo Tomas, Chile, on 28 December 2015. All patients signed an informed consent before the study, according to the Helsinki declaration and the norms revised by the Secretariat of the World Medical Association regarding the informed consent. The study is registered in the web ClinicalTRials.gov with number NCT03159312.
Measurement instruments
Bioimpedance has been used to measure body composition; in this case, it was carried out through the Tanita BC-418 MA. The patients were evaluated after an overnight fast, and according to the protocol established for this test. The BIA is based on the fact that lean tissue has more content of electrolytes and water than fat. This difference in electrolyte content permits estimating FFM, which measures the amount of electricity that flows through the body from the source to the electrodes (20). The BIA exam was evaluated by the same nutritionist professional on all opportunities, to diminish possible bias.
Grip strength was measured on both sides (dominant and non-dominant), with the same researcher in charge of all the tests, through a hydraulic hand dynamometer (Smedley Dynamometer, Spring, USA), according to recommendations by the American Association of Hand Therapists (21). Prior to using the hand dynamometer, it was adapted to the hand size, in a comfortable position for the patient. The patient was placed in upright position, with the shoulder adducted and rotating toward a neutral position; the arm extended, the forearm in neutral position and the wrist in slight extension (between 0 and 30°). Patients were asked to squeeze the dynamometer with the maximum force possible, through a brief maximum contraction and without performing additional body movements. Three tests were run with each hand, with one minute rest between each test, and the best score was used as the patient’s baseline strength (22).
Calculation of sample size
Sample size was calculated from changes based on grip strength measured via dynamometry in bariatric population (23), which proposes a difference of medians of 2.88 kg, with a standard deviation of 2.3 kg as the minimum difference required to obtain substantial clinical changes. The calculation yielded indicates that for each group at least 16 participants are required, considering a significance level of 0.05, 90 % statistical power, and an expected 15 % loss. The size selected should be increased by 15 % - 20 %, to prevent possible losses or withdrawals during follow up (Figure 1).
Figure 1. Flow diagram of the study participants through six months
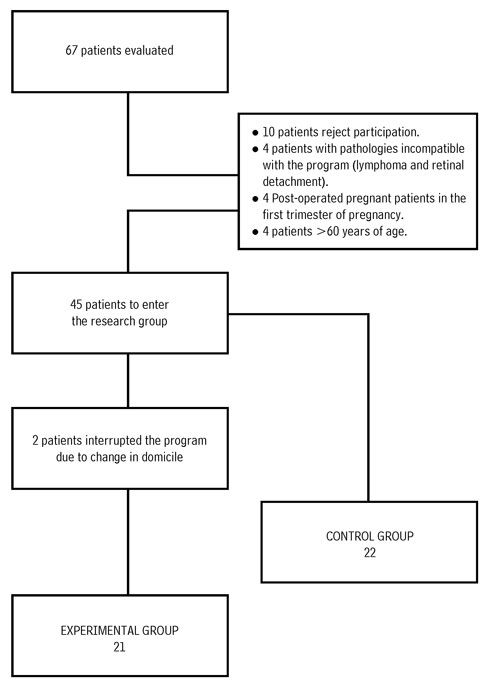
Source: Own elaboration.
Statistical analysis
Median differences were contrasted between each group for each variable and time separately. In this case, the study proceeded as with a descriptive study, calculating measures of central tendency and dispersion. Data normality was contrasted with the Shapiro-Wilkes test. To analyze the variables related, a bivariate analysis was performed by applying Student’s t test for the numerical variables, or the Mann-Whitney test in cases in which the normality hypothesis was not fulfilled. The significance value considered was p <0.05. The data were analyzed with the IBM SPSS Statistics 19 software. Statistical bias was controlled, given that the research was carried out with an experimental group and a control group.
Results
The study was held between March 2015 and March 2018, in the surgical specialization consultation at the Lircay Clinic, in the city of Talca, Chile. Attendance of the patients to the intervention program was at 80 %, after two from the IG abandoned the program because they lived too far. The IG attended 97 % of the programmed evaluations, and the CG to 100 %. The group, as a whole, was comprised of 32 women (74.4 %) and 11 men (25.6 %). The IG was constituted by 21 patients and the CG by 22. The mean age was 33 ± 6.9 years. The pre-operatory weight of the patients was 95.66 ± 13 and 103.04 ±14.4 kg in the intervention and control groups, respectively. The BMI was 35.5 ± 3.3 in the IG and 36.7 ± 3.3 in the CG. Upon evaluating grip strength in the baseline, the IG and CG had values of 34.19 kg and 34.18 kg, respectively. The values presented in Table 1 correspond to the pre-operatory (one month and six months prior to surgery).
Table 1. Description of the median and standard deviation of weight, BMI, and grip strength

Note: In parenthesis,
below the median, the standard deviation (SD) is shown.
Source: Own elaboration.
The BIA revealed an average amount of pre-operatory body fat of 44 kg. During the course of the study, the participants were able to reduce significantly their body fat; six months after surgery, they obtained an average loss of 23.9 kg of fat, which represents a reduction of 20 kg. The patients had a median pre-operatory LBM of 59 kg, and after six months obtained a measurement of 13.9 kg.
The baseline pre-operatory metabolism was at 1974, and diminished six months after the operation to 1331, with a difference of 642.21 (Table 2).

Note: In parenthesis,
below the median, the standard deviation (SD) is shown
Source: Own elaboration.
When running Student´s t test for independent samples in all the variables (weight, BMI, grip strength, LBM, FM, and metabolism), the result is that no significant differences exist between the IG and the CG with p > 0.05.
Discussion
The aim of the study was to determine the influence of an exercise program of moderate intensity on grip strength in patients operated of BS.
In relation to the withdrawal rate, 20 % of the sample selected stopped attending the training or the control. These values are below the figure estimated in the lack of adherence to programs of physical activity and post-surgical control (60 % - 70 % withdrawal) (24) .
This study coincides with research that reveals that women undergo BS with greater frequency. According to the findings, idealization of the female body leads women to intervene their bodies, as well as other factors: Difficulty to lose weight after pregnancy, poor habits, and lack of physical activity (25).
The moderate exercise program produced weight loss, after six months, of 28.53 % of the initial weight, and both groups had an important loss after the third month. These results are similar to the studies by Coleman et al., (18) and Trofa et al., (26) who found a positive correlation between post-operatory physical activity and the degree of weight loss, as well as a significant difference in weight loss between active and inactive groups. These studies also relate pre-operatory BMI with regaining weight in the long term, but Metcalf et al., conclude that no difference exists in weight loss between the exercise group and those who do not engage in exercise, although there is decreased FM and LGM during the first months (p < 0.05) (27).
Regarding that reported by Stegen et al., static muscle strength, measured as grip strength, establishes that such diminished by 18 % and 7 % in the control group and in the experimental group, respectively, four months after undergoing BS (28). In turn, the study by Hassannejad et al., shows that no changes were evident in muscle strength or in the composition of LBM, but that there was an important increase in aerobic capacity in the IG (9). The sample in this study presents similar results, given that although the IG conducted specific muscular work, LBM decreased, a result that can be attributed to low intake of proteins due to the post-operative diet and, thereby, to the loss of FM and LBM. Another study demonstrated that although patients with morbid obesity experienced a significant loss of muscle strength after surgery, their body could easily adapt to this change because of the loss of body weight in relation to even reduced strength (29). A study subjecting eight patients who had undergone BS to training with strength exercises prescribed discovered that, although the loss of mass without fat is inevitable, post-operatory exercise programs may not only preserve muscle strength, but also a significant impact on the increase of the dynamic strength of the majority of muscles. According to the study by Huck, 12 weeks of supervised resistance training improved functional strength (sitting and standing test), both in the CG as in the IG, and there was certain progression in flexibility and grip strength, but without significant changes (30). The study conducted by our research group lasted 24 weeks, with similar results to those of the study mentioned, which supposes that the exercise time should increase in weeks of exercise.
Finally, a study described that pre-operatory grip strength is directly related with post-operatory body composition. The importance of this study lies in being able to supervise the evolution of patients in which grip strength diminishes and, hence, LBM. These results agree with those from this research, which demonstrated the post-operatory decrease of muscle mass and grip strength, in spite of the component of physical exercise (23).
Study limitations
Patient attendance to the intervention program was at 80 %, given that some withdrew from the program because they lived far away, and the sample size, although having a significance level of 0.05, was only comprised of 43 patients. Nevertheless, it is observed that physical exercise has indeed been effective in reducing weight and maintaining such in the medium term, without rebound effect.
Conclusions
A moderate physical activity program lasting six months in patients intervened for BS has no significant results in the development of muscle mass evaluated through hand dynamometry. However, physical exercise has been effective in lowering weight and in maintaining such in the medium term, without rebound effect.
We recommend continuing with the physical activity intervention program to prevent regaining weight in these patients, which tends to take place after two years, according to other studies conducted. The nursing care prescribed includes taking the patients’ weights, stimulating them into performing the exercises in routine manner, offering them information on managing an adequate diet, and educating the family (or the environment) so that it contributes in the patient’s adaptation process, given that post-operatory care is essential.
Having carried out the intervention program, improved quality of life of the patients has been proven, upon diminishing the limitations produced by the excess weight.
Conflict of interest: None declared.
Funding: The study has not received external funding.
References
1. Eduardo-Atalah S. Epidemiología de la obesidad en Chile. Revista Médica Clínica Las Condes. [2012 Mar. 1]; 23(2):117-23. DOI: 10.1016/S0716-8640(12)70287-0
2. Delgado-Floody P, Caamaño-Navarrete F, González-Rivera J, Fleckenstein J, Banzer W, Martínez-Salazar C. Improvements in Chilean patients with obesity following a 5-month multidisciplinary exercise program: A feasibility study. J Sports Med Phys Fitness. [2018 Mar.]; 58(3):309-17. DOI: 10.23736/S0022-4707.17.06839-6
3. Malo-Serrano M, Castillo MN, Pajita DD. La obesidad en el mundo. Anales de la Facultad de Medicina. 2017;78:173-8. DOI: 10.15381/anales.v78i2.13213
4. Valle-Leal J, Abundis-Castro L, Hernández-Escareño J, Flores-Rubio S. Índice cintura-estatura como indicador de riesgo metabólico en niños. Revista chilena de pediatría. 2016;87:180-5. DOI: 10.1016/j.rchipe.2015.10.011
5. Engin A. The definition and prevalence of obesity and metabolic syndrome. In: Engin AB, Engin A, editors. Obesity and Lipotoxicity. Cham: Springer International Publishing; 2017. p. 1-17. DOI: 10.1007/978-3-319-48382-5_1
6. Wakamatsu K, Seki Y, Kasama K, Uno K, Hashimoto K, Seto Y, et al. Prevalence of Chronic Kidney Disease in Morbidly Obese Japanese and the Impact of Bariatric Surgery on Disease Progression. Obesity Surgery. [2018 Feb. 1]; 28(2):489-96. DOI: 10.1007/s11695-017-2863-7
7. Coimbra S, Reis F, Ferreira C, Nunes S, Viana S, Catarino A, et al. Weight loss achieved by bariatric surgery modifies high-density lipoprotein sub-fractions and low-density lipoprotein oxidation towards atheroprotection. Clinical Biochemistry. [2019 Jan. 1]; 63:46-53. DOI: 0.1016/j.clinbiochem.2018.10.007
8. Takemoto E, Wolfe BM, Nagel CL, Boone-Heinonen J. Reduction in comorbid conditions over 5 years following bariatric surgery in medicaid and commercially insured patients. Obesity. 2018;26(11):1807-14. DOI: 10.1002/oby.22312
9. Hassannejad A, Khalaj A, Mansournia MA, Rajabian-Tabesh M, Alizadeh Z. The effect of aerobic or aerobic-strength exercise on body composition and functional capacity in patients with BMI ≥35 after bariatric surgery: A randomized control trial. Obesity Surgery. [2017 Nov. 1]; 27(11):2792-801. DOI: 10.1007/s11695-017-2717-3
10. Al-Khyatt W, Ryall R, Leeder P, Ahmed J, Awad S. Predictors of inadequate weight loss after laparoscopic gastric bypass for morbid obesity. Obesity Surgery. [2017 jun. 1]; 27(6):1446-52. DOI: 10.1007/s11695-016-2500-x
11. Kerstyn C. Zalesin MD, Barry A. Franklin PD, Martin A. Lillystone MA, Tania-Shamoun MD, Kevin R. Krause MD, David L. Chengelis MD, et al. Differential loss of fat and lean mass in the morbidly obese after bariatric surgery. Metabolic Syndrome and Related Disorders. 2010;8(1):15-20. DOI: 10.1089/met.2009.0012
12. Sánchez-Ortega L, Sánchez JC, García A. Valoración de un programa de ejercicio físico estructurado en pacientes con obesidad mórbida pendientes de cirugía bariátrica. Nutricion hospitalaria. 2014;29:64-72. DOI: 10.3305/nh.2014.29.1.6937
13. Maïmoun L, Lefebvre P, Jaussent A, Fouillade C, Mariano-Goulart D, Nocca D. Body composition changes in the first month after sleeve gastrectomy based on gender and anatomic site. Surgery for Obesity and Related Diseases. [2017 May. 1]; 13(5):780-7. DOI: 10.1016/j.soard.2017.01.017
14. Schiavo L, Scalera G, Pilone V, De Sena G, Iannelli A, Barbarisi A. Fat mass, fat-free mass, and resting metabolic rate in weight-stable sleeve gastrectomy patients compared with weight-stable non-operated patients. Surgery for Obesity and Related Diseases. [2017 Oct. 1]; 13(10):1692-9. DOI: 10.1016/j.soard.2017.06.007
15. Nicoletti CF, Camelo JS, Dos Santos JE, Marchini JS, Salgado W, Nonino CB. Bioelectrical impedance vector analysis in obese women before and after bariatric surgery: Changes in body composition. Nutrition. [2014 May 1]; 30(5):569-74. DOI: 10.1016/j.nut.2013.10.013
16. Schaap LA, Fox B, Henwood T, Bruyère O, Reginster JY, Beaudart C, et al. Grip strength measurement: Towards a standardized approach in sarcopenia research and practice. European Geriatric Medicine. [2016 Jun. 1]; 7(3):247-55. DOI: 10.1016/j.eurger.2015.11.012
17. Scott D, Hirani V. Sarcopenic obesity. European Geriatric Medicine. [2016 Jun. 1]; 7(3):214-9. DOI: 10.1016/j.eurger.2015.11.009
18. Coleman KJ, Caparosa SL, Nichols JF, Fujioka K, Koebnick C, McCloskey KN, et al. Understanding the capacity for exercise in post-bariatric patients. Obesity Surgery. [2017 Jan. 1]; 27(1):51-8. DOI: 10.1007/s11695-016-2240-y
19. Herring LY, Stevinson C, Carter P, Biddle SJH, Bowrey D, Sutton C, et al. The effects of supervised exercise training 12-24 months after bariatric surgery on physical function and body composition: A randomized controlled trial. International Journal of Obesity. [2017 Mar. 6]. DOI: 10.1038/ijo.2017.60
20. Widen EM, Strain G, King WC, Yu W, Lin S, Goodpaster B, et al. Validity of bioelectrical impedance analysis for measuring changes in body water and percent fat after bariatric surgery. Obesity Surgery. [2014 Jun. 1]; 24(6):847-54. DOI: 10.1007/s11695-014-1182-5
21. Wichelhaus A, Harms C, Neumann J, Ziegler S, Kundt G, Prommersberger KJ, et al. Parameters influencing hand grip strength measured with the manugraphy system. BMC Musculoskeletal Disorders. [2018 Feb. 14]; 19(1):54. DOI: 10.1186/s12891-018-1971-4
22. Mühldorfer-Fodor M, Ziegler S, Harms C, Neumann J, Kundt G, Mittlmeier T, et al. Load distribution of the hand during cylinder grip analyzed by Manugraphy. Journal of Hand Therapy. [2017 Oct. 1]; 30(4):529-37. DOI: 10.1016/j.jht.2016.10.009
23. Otto M, Kautt S, Kremer M, Kienle P, Post S, Hasenberg T. Handgrip strength as a predictor for post bariatric body composition. Obesity Surgery. [2014 Dec. 1]; 24(12):2082-8. DOI: 10.1007/s11695-014-1299-6
24. Campanha-Versiani L, Pereira DAG, Ribeiro-Samora GA, Ramos AV, De Sander-Diniz MFH, De Marco LA, et al. The effect of a muscle weight-bearing and aerobic exercise program on the body composition, muscular strength, biochemical markers, and bone mass of obese patients who have undergone gastric bypass surgery. Obesity Surgery. [2017 Aug. 1]; 27(8):2129-37. DOI: 10.1007/s11695-017-2618-5
25. Sellberg F, Willmer M, Tynelius P, Berglind D. Four years’ follow-up changes of physical activity and sedentary time in women undergoing roux-en-Y gastric bypass surgery and appurtenant children. BMC Surgery. [2017 Dec. 11]; 17(1):133. DOI: 10.1186/s12893-017-0318-7
26. Trofa D, Smith EL, Shah V, Shikora S. Total weight loss associated with increased physical activity after bariatric surgery may increase the need for total joint arthroplasty. Surgery for obesity and related diseases. [2014 Mar. 1]; 10(2):335-9. DOI: 10.1016/j.soard.2013.09.011
27. Metcalf B, Rabkin RA, Rabkin JM, Metcalf LJ, Lehman-Becker LB. Weight loss composition: The effects of exercise following obesity surgery as measured by bioelectrical impedance analysis. Obesity Surgery. [2005 Feb. 1];15(2):183-6. DOI: 10.1381/0960892053268381
28. Stegen S, Derave W, Calders P, Van Laethem C, Pattyn P. Physical fitness in morbidly obese patients: Effect of gastric bypass surgery and exercise training. Obesity Surgery. [2011 Jan. 1]; 21(1):61-70. DOI: 10.1007/s11695-009-0045-y
29. Hue O, Berrigan F, Simoneau M, Marcotte J, Marceau P, Marceau S, et al. Muscle force and force control after weight loss in obese and morbidly obese men. Obesity Surgery. [2008 Sept. 1]; 18(9):1112-8. DOI: 10.1007/s11695-008-9597-5
30. Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial–a prospective controlled intervention study of bariatric surgery. Journal of Internal Medicine. 2013; 273(3):219-34. DOI: 10.1111/joim.12012