Article
Carolina Marques de
Almeida 1
Camila Fernandes Pollo 2
Silmara Meneguin 3
1 ![]() 0000-0002-7872-8558. Intensive Care Unit, Universidade Estadual
Paulista, Brazil.
0000-0002-7872-8558. Intensive Care Unit, Universidade Estadual
Paulista, Brazil.
2 ![]() 0000-0003-0264-5841. Department of Nursing, Universidade Estadual
Paulista, Brazil.
0000-0003-0264-5841. Department of Nursing, Universidade Estadual
Paulista, Brazil.
3 ![]() 0000-0003-3853-5134. Department of Nursing, Universidade Estadual
Paulista, Brazil. s.meneguin@unesp.br
0000-0003-3853-5134. Department of Nursing, Universidade Estadual
Paulista, Brazil. s.meneguin@unesp.br
Received: 07/05/2019
Sent to peers: 09/06/2019
Approved by peers: 15/08/2019
Accepted: 09/09/2019
Theme: evidence-based practice.
Contribution to the discipline: this study provides subsidies for a safe nursing practice, based on scientific evidence, which may support the implementation of more purposeful intervention models for nurses working in intensive care units. Moreover, the findings of this study could be used by these professionals to reflect on the professional practice, which contributes to the care offer consistent with the needs of each patient. It also encourages future research on this theme, with new approaches to the qualification of critical patient care.
To reference this article / Para citar este artículo / Para citar este article: de Almeida CM, Pollo CF, Meneguin S. Nursing Interventions for Patients with Intracranial Hypertension: Integrative Literature Review. Aquichan 2019; 19(4): e1949. DOI: https://doi.org/10.5294/aqui.2019.19.4.9
|
Abstract Objective: the study sought to identify, in national and international
publications, the principal Nursing interventions aimed at patients with
intracranial hypertension. Keywords (Source DeCS): Hemodynamic monitoring; intracranial pressure; nursing care management; nursing care; nursing. |
Resumen Objetivo: el estudio tiene como
objetivo identificar, en publicaciones nacionales e internacionales, las
principales intervenciones de Enfermería dirigidas a pacientes con hipertensión
intracraneal. Palabras clave (Fuente: DeCS): Monitorización hemodinámica; presión intracraneal; cuidados de enfermería; atención de enfermería; enfermería. |
Resumo Objetivo: este estudo
objetiva identificar, nas publicações nacionais e internacionais, as principais
intervenções de Enfermagem direcionadas a pacientes com hipertensão
intracraniana. Palavras-chave (Fonte DeCS): Monitorização hemodinâmica; pressão intracraniana; cuidados de enfermagem; assistência de enfermagem; enfermagem. |
Introduction
Intracranial pressure (ICP) is an event of great clinical repercussion that attacks patients with brain tumors, severe brain injury, and extensive ischemic and hemorrhagic cerebral vascular accident. Increased ICP is a major cause of secondary cerebral lesion and is frequently associated with worsened neurological evolution (1-3).
Conceptualized as cerebrospinal fluid (CSF) pressure from blood and brain tissue pressure, normal values range from 5 to 15 mmHg. (4). In critically ill patients, ICP may vary due to changes in blood pressure, ventilation, patient positioning, as well as changes in carbon dioxide and oxygen pressures (5). Increased ICP, above 20 mmHg, has as an important physiological repercussion in the reduction of cerebral perfusion pressure and cerebral blood flow, in addition to compressing brain structures and contributing to hydrocephalus, besides causing brain herniation (6-9).
Intracranial pressure monitoring by implanting a polyethylene catheter into the ventricular cavity connected to a pressure transducer is critical to prevent secondary brain damage that contributes to increased morbidity and mortality (10-13). Despite being an invasive procedure that involves health and safety risks to those who use it, it is the only accepted method for the safe diagnosis of increased ICP, as well as for its treatment in some clinical situations (14-16).
Added to the control of clinical, hemodynamic, respiratory, and metabolic parameters, monitoring the ICP helps and guides the therapy of neurological patients, as it allows for its rapid recognition and permits assessing the therapeutic efficacy, as well as brain injury (17-18).
Although catheter insertion is an inherent procedure for the neurosurgery team, its care and ICP monitoring are the responsibilities of the intensive care unit (ICU) nursing staff (19).
In addition, it should be considered that the nurse is the bedside professional giving meaning to the ICP monitoring parameters, through theoretical knowledge, logical reasoning, and experience acquired in practice (20). Care consistent with knowledge and practices combined with educational and care actions in the professional practice to ensure the quality of care provided to neuro-critical patients (21).
In the ICU, Nursing professionals should avoid unnecessary harm during health care delivery to improve the care provided and prevent iatrogenesis (22-23). Iatrogenic events, within this context, may put patient at risk of life and bring complications that may compromise their clinical course and safety (24).
It should be noted that increased ICP often occurs as a result of routine nursing procedures, such as bed bath, patient positioning, and oral and bronchial hygiene, among others (25-26). In this sense, the nursing staff should be aware of signs and symptoms of worsening intracranial hypertension, which depend on the location of the brain injury. However, the most common symptom is worsening mental state (27-29).
In this sense, systematization of Nursing care (SNC) is an important tool, given that it permits the Nursing staff to organize and direct their practice to the specific needs of each patient and prevent unnecessary harm (30).
Considering that the quality of health care is linked to the incorporation of good nursing practices, this study sought to know the interventions directed to patients with ICP monitoring to contribute to care based on scientific principles and the best evidence.
The objective of this study was to identify, in national and international publications, the principal Nursing interventions aimed at patients with intracranial hypertension.
Materials and Methods
Integrative literature review, conducted in five stages: problem identification, literature search, data evaluation, data analysis, and presentation of integrative review or synthesis of knowledge (31-32). To conduct this study, the following question was used: “What nursing interventions are described in the scientific literature for patients with intracranial hypertension?”
To search for the articles, on-line access was used to the following databases: Latin American and Caribbean Literature in Health Sciences (LILACS, for the term in Spanish), PubMed, Scopus, Web of Science, Cinahal, and Google Scholar. The descriptors selected from the list of Health Sciences Descriptors (DeCS) were: “hemodynamic monitoring”, “intracranial pressure”, “Nursing care” and “Nursing assistance”, “Nursing interventions”, “neuro-intensive care”, with Boolean operators OR and AND.
The search was carried out in December 2018. To include the articles, the following criteria were considered: original articles that addressed the guiding question, published between 2013 and 2018, in Portuguese, English, and Spanish. Articles not available in full, experience reports, literature reviews, theses and dissertations were excluded.
In order to obtain more accurate results, the search was aided by two researchers involved in the study. For the data collection of the studies, an instrument was elaborated that included the following information: year of publication, authors, objective, country in which the study was carried out, database, research design, sample detailing, intervention, results and recommendation/conclusions. Such information contributed to the analysis and synthesis of the data obtained in the search.
Results
The study initially identified 630 articles; of these, 380 were excluded because they were duplicated in the databases. Thus, 250 articles were selected to read the title and abstract, which resulted in a sample of 50 articles for full-text reading. Of these, 43 were excluded for not answering the guiding question, which lead to a total of seven articles (Figure 1). Four studies were conducted in the United States, two in Europe, and one in Brazil.
Figure 1. Selection process of articles in the integrative review (Botucatu, Brazil, 2019)
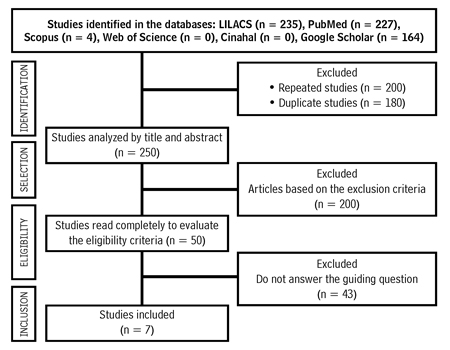
Source: Own elaboration.
Table 1 presents the characteristics of the articles selected for this review, according to author, year of publication, database, research design, and results associated to Nursing interventions.
Table 1. Articles included in the study according to title, author, place, year of publication, databases and countries of origin, research design and main results and interventions (Botucatu, Brazil, 2019)
Author/year/research location/database |
Article title |
Research design |
Results associated with Nursing interventions |
Article 1 Rosa NM, Lima JF, Inoue KC, 2013 (33), Brazil, LILACS |
Knowledge of Nursing staff on neuro-intensivism and the influence of continuing education |
Descriptive, exploratory, and quantitative study, which sought to characterize the knowledge of the Nursing staff on neuro-intensivism. |
• Normality parameters of CPP, MBP, CVP, SvJO2, ETCO2, ICP. • Parameters to note for patient assessment. • Nursing care after patient manipulation. • Aspiration of endotracheal tube. • Mathematical representation of parameters to calculate CPP. • Factors and/or procedures that contribute to elevation of ICP. |
Article 2 Uğraş GA, Yüksel S, Temiz Z et al., 2018 (34), The United States of America, PubMed |
Effects of different head-of-bed elevations and body positions on intracranial pressure and cerebral perfusion pressure in neurosurgical patients |
Quasi experimental study. |
The study showed that different patient and headboard positions led to insignificant changes in ICP and CPP. |
Article 3 Sacco TL, Delibert, SA, 2018 (35), The United States of America, PubMed |
Management of intracranial pressure: Part I |
Descriptive study. |
Nursing care for these patients includes collaboration with an inter-professional staff and is oriented at patient and family comfort. The use of a guideline based on evidence to manage ICP is strongly encouraged to improve the results of patients. |
Article 4 Nyholm L, Steffansson E, Frojd C et al., 2014 (36), Sweden, PubMed |
Secondary injuries related to nursing interventions in neuro-intensive care: a descriptive pilot study |
Prospective, observational study that aimed to investigate events secondary to oral hygiene, bed mobilization, endotracheal aspiration, hygiene measures, and simultaneous neuro-intensive care interventions. |
The most common type of event after Nursing care was increased ICP, followed by low cerebral perfusion pressure and mean blood pressure. |
Article 5 Robinson JD, 2015 (37), The United States of America, PubMed |
Management of refractory intracranial pressure |
Descriptive article that addresses the approaches to treat brain injury and emphasizes the role of nursing in controlling ICP. |
• Safe airway. • Maintain eucapnia. • Avoid hypotension. • MBP > 90mmHg. • Maintain glycemia levels between 80 and 180 mg/dl. • Maintain temperature at 37 °C. • Adequate sedation. • Maintenance of bed elevation at 30 degrees. • Maintain head neutral (aligned with the body). • When using a cervical collar, two fingers should fit inside the collar. • Medications used to control ICP: mannitol 20 % and hypertonic saline solution. • For decreased brain metabolism, barbiturates or hypothermia. The authors emphasize the role of nursing in hypotension control after pentobarbital bolus. Hypothermia (32 to 34 °C) reduces ICP for 24 to 72 h. • Recognition of signs of brain herniation: asymmetrical, non-reactive pupils, decortication or decerebration posture, bradycardia hypertension and respiratory arrest. |
Article 6 Szabo CM, Grap, MJ, Starkweather A et al., 2014 (38), The United States of America, PubMed |
The Effect of oral care on intracranial pressure in critically Ill adults |
Observational, non-experimental study, which sought to investigate the effects of care of oral hygiene on ICP. |
The repeated-measures mixed-effect variance analysis model indicated a statistically significant increase in ICP in response to oral hygiene (p = 0.0031). However, there was no clinically significant effect on ICP. This study provides evidence that oral hygiene is safe for patient performance in the absence of pre-existing elevated ICP. |
Article 7 Nyholm L, Howells T, Enblad P, 2017 (25), Sweden, PubMed |
Predictive factors that may contribute to secondary injury with nursing interventions in adults with traumatic brain injury |
Prospective, quantitative study seeking to investigate the risk of inducing high intracranial pressure related to nursing interventions.. |
Increase of secondary ICP related to nursing interventions occurring in six patients (21 %) and eight occasions (12 %). Patients with baseline ICP of 15 mmHg or more present risk 4.7 times higher of developing an injury. The initial ICP of 15 mm Hg or more was the most important factor to determine the risk of injury secondary to ICP. |
CPP — Cerebral Perfusion Pressure; MBP — Mean Blood
Pressure; CVP — Central Venous Pressure; SvJO2 — Jugular Bulb Oximetry;
ETCO2 — CO2 at the end of expiration.
Source: Own elaboration.
Figure 2 shows the structural synthesis of nursing interventions identified in the literature (Botucatu, Brazil, 2019).
Figure 2. Structural synthesis of the Nursing interventions (Botucatu, Brazil 2019)
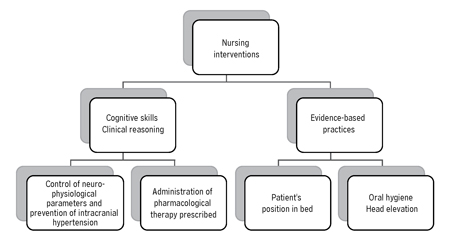
Source: Own elaboration.
The reading and analysis of the articles permitted observing that the Nursing interventions are linked to cognitive skills and clinical reasoning, but they should also be supported by practices based on the best scientific evidence.
The nurse’s cognitive skills and clinical reasoning are fundamental to interpret the neuro-physiological and hemodynamic parameters, prevent the increase of ICP during Nursing procedures, and administer the pharmacological therapy prescribed. However, it is in evidence-based practice (EBP) that care has the scientific support needed to improve care practice.
Discussion
Caring for patients with neurological alterations is a big challenge for the whole Nursing staff. Patients with ICP require specific and continuous care in ICU and demand maximum attention from the health staff and minimum manipulation, in order to avoid possible deleterious injuries or aggravate those existing (20, 39-41).
As prerequisite to monitor ICP, the nurse needs to be aware of the principles of monitoring, neuro-anatomy, and neurophysiology, as well as the pathophysiology of intracranial hypertension (ICH) (42). It is known that increased ICP may be associated with the patient’s clinical condition or may occur in response to routine Nursing care. Therefore, the focus of medical and nursing interventions should be the prevention or minimization of secondary brain injury (37, 43-44).
A study conducted with 18 patients with neurosurgical diagnoses revealed that the most common types of secondary events after Nursing care were increased intracranial pressure, followed by a fall in cerebral perfusion pressure and mean blood pressure. The authors concluded that patients with increased risk of secondary events must be recognized and their care and treatment must be rigorously planned (36).
In this sense, the literature emphasizes the importance of Nursing empowerment in the multidisciplinary staff and the use of care protocols that include interventions to control and manage ICP to intervene briefly and effectively in treatments aimed at mitigating this event, as well as adjusting nursing procedures that, by association, may increase intracranial hypertension and decrease cerebral perfusion pressure (25-27).
In the survey conducted in this research, it was identified that nursing interventions are linked to cognitive skills and clinical reasoning, essential to interpret the monitoring parameters and implement care to control ICP.
The interventions described in the literature found during the search period are neuro-physiological and encompass monitoring of hemodynamic parameters, like oxygen saturation, mean blood pressure, temperature, ICP, and cerebral perfusion pressure.
This search identified two works that describe procedures that, indirectly, can contribute to increase ICP and whose scientific evidence supports the best care. One of the procedures is the elevation of the bed headboard and the body position. Although the only study that addressed the subject did not find a statistically significant change in ICP values with the bed headboard at 15, 30, and 45 degrees, as well as in the supine, right, and left lateral positions, the sample size of 30 patients was considered a research limitation (34). However, other investigations show that patients with increased ICP benefit from head elevation by 10, 15, 30, and 45 degrees compared to zero degrees (45-46).
The other procedure described in the literature that contributed to increasing ICP is oral hygiene. A study that analyzed the influence of this procedure in 23 patients with ICP monitoring showed statistically significant increase of this parameter during oral hygiene (p = 0.0031), but without clinical repercussion (38).
Although this review did not include the inclusion of articles on endotracheal aspiration, it is essential to contextualize this procedure, which may also lead to increased ICP. A clinical study aimed at determining the best aspiration technique (open versus closed system) with 32 neurosurgical patients, showed that patients aspirated with open system had significantly lower mean carbon dioxide partial pressure than those aspirated with closed system, but without significant difference (47-50).
A recent study concluded that while most articles show an increase in ICP above 20 mmHg, when using the open aspiration system, it is still unclear which is the best technique to maintain adequate cerebral perfusion pressure. For the authors, more studies are necessary to determine the best endotracheal aspiration technique for the Nursing practice (51-52).
Implementing EBP-based care is critical to achieving effectiveness, reliability, and safety in health practices (53-54). In this context, nurses play an important role in planning the care for neuro-critical patients, given that they require daily systematized evaluation (35, 54).
Nurses should be very cautious, given that routine procedures can aggravate the neurological condition due to the increase in ICP and decrease in cerebral perfusion pressure. Therefore, professionals must be trained to provide safe and qualified care to critically ill patients, given the need for constant attention in the application of interventions for their recovery (20, 33, 55-59).
Thus, the neurological assessment is essential to identify Nursing diagnoses, a crucial stage to elaborate a care plan based on a theoretical framework, which guides and improves the practice, as well as directs nursing interventions and expected results (60-61). In addition, the underlying clinical decision to care is paramount to the quality and excellence of the nursing practice in neuroscience (62).
A limitation of this research was that of obtaining studies with small sample sizes; therefore, it is necessary to develop more robust studies on the theme.
Conclusions
Intracranial hypertension is an event of great clinical impact. Complications arising from this event can be minimized and controlled through specific nursing interventions that include controlling neuro-physiological and hemodynamic parameters, as well as preventing the increase of ICP, often linked to the performance of nursing procedures.
The results of this study also evidence the importance of the best evidence-based care practice to support the multifaceted care that neurological patients require in ICU and whose success depends on a cohesive inter-professional staff, which also recognizes the family as an integral part of health care.
Despite the number of publications on the pathophysiology, it was found that few studies address Nursing care to the family and the patient affected by this secondary lesion, which may evolve to death.
Conflict of interest: none declared.
References
1. Le Roux P, Menon DK, Citerio G, Vespa P, Bader MK, Brophy G et al. The international multidisciplinary consensus conference on multimodality monitoring in neurocritical care: evidentiary tables: a statement for healthcare professionals from the neurocritical care Society and the European society of intensive care medicine. Neuro crit Care. 2014;21(2):297-361. DOI: https://doi.org/10.1007/s12028-014-0081-x
2. Chesnut R, Videtta W, Vespa P, Le Roux P. Participants in the International Multidisciplinary Consensus Conference on Multimodality Monitoring. Intracranial pressure monitoring: fundamental considerations and rationale for monitoring. Neuro crit Care. 2014;21(Suppl 2):S64-84. DOI: https://doi.org/10.1007/s12028-014-0048-y
3. Lantigua H, Gutierrez SO, Schmidt JM, Lee K, Badjatia N, Agarwal S et al. Subarachnoid hemorrhage: who dies, and why? Critical Care. 2015; 19:309. DOI: https://doi.org/10.1186/s13054-015-1036-0
4. Olson DM, Lewis LS, Bader MK et al. Significant practice pattern variations associated with intracranial pressure monitoring. J Neurosci Nurs 2013;45(4):186-93. DOI: https://doi.org/10.1097/JNN.0b013e3182986400
5. Tang A, Pandit V, Fennell V, Jones T, Joseph B, O’Keeffe T et al. Intracranial pressure monitor in patients with traumatic brain injury. J Surg Res. 2015 [Epub 2014 Nov 18];194:565-70. DOI: https://doi.org/10.1016/j.jss.2014.11.017
6. Graham DI. Pathology of brain damage after head injury. Head injury. 2000 [Epub 2019 Sept 12]:176-94. Available from: https://www.researchgate.net/publication/313441655_Pathology_of_brain_damage_after_head_injury
7. American Association of Neuroscience nurses. Nursing management of adults with severe traumatic brain injury. Glenview (IL): AANN Clinical Practice Guidelines. 2008:1-20.
8. Hemphill III JC, Rabinstein, Samuels OB, editors. The practice of neurocritical care. Kindle edition; Kindle locations 3375-3378. Minneapolis (MN): Neurocritical Care Society; 2015.
9. Smeltzer SC, Bare BG. Brunner & Suddarth: tratado de enfermagem médico-cirúrgica. 15a ed. Rio de Janeiro: Guanabara Koogan; 2015.
10. Chesnut RM, Bleck TP, Citerio G, Classen J, Cooper DJ, Coplin WM et al. A consensus-based interpretation of the benchmark evidence from South American trials: treatment of intracranial pressure trial. J Neurotrauma. 2015 [Epub 2015 Aug 31];32(22):1722-4. DOI: https://doi.org/10.1089/neu.2015.3976
11. Olson DM, Andrew KW, O’Phelan K, Gupta PK, Figueroa SA, Suarez JI. Global Monitoring in the Neurocritical Care Unit. Neurocritical Care. 2015;22(3):337-47. DOI: https://doi.org/10.1007/s12028-015-0132-y
12. Rogers M, Stutzman SE, Atem FD, Sengupta S, Welch B, Olson DM. Intracranial Pressure Values Are Highly Variable After Cerebral Spinal Fluid Drainage. J Neurosci Nurs. 2017;49(2):5-9. DOI: https://doi.org/10.1097/JNN.0000000000000257
13. Kawoos U, McCarron RM, Auker CR, Chavko M. Advances in Intracranial Pressure Monitoring and Its Significance in Managing Traumatic Brain Injury. Int J Mol Sci. 2015;16(12):28979-97. DOI: https://doi.org/10.3390/ijms161226146
14. Castillo LR, Gopinath S, Robertson CS. Management of intracranial hypertension. Neurologic Clinics. 2008;26(2):521-41. DOI: https://doi.org/10.1016/j.ncl.2008.02.003
15. Dang Q, SimonJ, Catino J, Puente I, Habib F, Zucker L, Bukur M. More fateful than fruitful? Intracranial pressure monitoring in elderly patients with traumatic brain injury is associated with worse outcomes. J Surg Res. 2015;198(2):482-8. DOI: https://doi.org/10.1016/j.jss.2015.03.092
16. Silva JA, Souza AR, Feitoza AR, Cavalcante TMC. Traumatismo cranioencefálico no município de Fortaleza. Enferm Foco 2017;8(1):22-6. DOI: https://doi.org/10.21675/2357-707X.2017.v8.n1.724
17. Hickey JV, Olson D, Turner D. Intracranial pressure waveform analysis during rest and suctioning. Biol Res Nurs. 2009 [Epub 2009 Apr 26];11:174-96. DOI: https://doi.org/10.1177/1099800409332902
18. Hirzallah MI, Choi HÁ. The Monitoring of Brain Edema and Intracranial Hypertension. J Neurocrit Care. 2016;9(2):92-104. DOI: https://doi.org/10.18700/jnc.160093
19. Heck C. Invasive Neuromonitoring. Crit Care Nurs Clin North Am. 2016 [Epub 2015 Dec 17];28(1):77-86. DOI: https://doi.org/10.1016/j.cnc.2015.10.001
20. Alcântara TFDL, Marques IR. Avanços na monitorização neurológica intensiva: implicações para a enfermagem. Rev Bras Enferm. 2009;62(6):894-900. DOI: http://dx.doi.org/10.1590/S0034-71672009000600015
21. Venturi V, Viana CP, Maia LFM, Basílio MJ, Oliveira AO, Sobrinho JC et al. O papel do enfermeiro no manejo da monitorização hemodinâmica em unidade de terapia intensiva. Recien. 2016;6(17):19-23. DOI: https://doi.org/10.24276/rrecien2358-3088.2016.6.17.19-23
22. Pedreira ML. Práticas de enfermagem baseadas em evidências para promover a segurança do paciente. Rev Acta Paul Enferm. 2009 [Epub 12 Sept. 2019];22(spe):880-1. Available from: http://www.scielo.br/pdf/ape/v22nspe/07.pdf
23. Nogueira LS, Padilha KG, Silva DV, Lança EFC, Oliveira EM, Sousa RMC. Pattern of nursing intervention performed on trauma victims according to the nursing activities score. Rev Esc Enferm USP. 2015;49(spe):28-34. DOI: http://dx.doi.org/10.1590/S0080-623420150000700005
24. Padilha KG, Kitahara PH, Gonçalves CC, Sanches AL. Ocorrências iatrogênicas com medicação em unidade de terapia intensiva: condutas adotadas e sentimentos expressos pelos enfermeiros. Rev Esc Enferm USP. 2002;36(1):50-7. DOI: http://dx.doi.org/10.1590/S0080-62342002000100008
25. Nyholm L, Howells T, Enblad P. Predictive Factors That May Contribute to secondary insults with nursing interventions in adults with traumatic brain injury. J Neurosci Nurs. 2017;49(1):49-55. DOI: https://doi.org/10.1097/JNN.0000000000000260
26. McNett MM, Olson DM. Evidence to guide nursing interventions for critically ill neurologically impaired patients with ICP monitoring. J Neurosci Nurs 2013;45(3):120-3. DOI: https://doi.org/10.1097/JNN.0b013e3182901f0a
27. Mendaro ARAD, Luna OC, Pérez LCA, Rodríguez MA. Caracterización epidemiológica y neurológica del traumatismo craneoencefálico frontal durante cinco años en Villa Clara. Medicent Electrón. 2017 [Epub 12 Sept. 2019];21(1):30-8. Available from: http://www.medicentro.sld.cu/index.php/medicentro/article/view/2145
28. McNett MM, Gianakis A. Nursing Interventions for Critically ill Traumatic Brain Injury Patients. J Neurosci Nurs. 2010;42(2):71-7. DOI: https://doi.org/10.1097/JNN.0b013e3181ce5b8a
29. Bulechek GM. Nursing Intervention Classification (NIC). 6th ed. St. Louis: Mosby Elsevier; 2016.
30. Conselho Federal de Enfermagem. Resolução n. 358, de 15 de outubro 2009. Dispõe sobre a sistematização da assistência de enfermagem e a implementação do processo de enfermagem em ambientes públicos ou privados em que ocorre o cuidado profissional de enfermagem e dá outras providências. Rio de Janeiro: Cofen; 2009.
31. Whittemore R, Knaft K. The integrative review: update methodology. J Adv Nurs. 2005;52(5):546-53. DOI: https://doi.org/10.1111/j.1365-2648.2005.03621.x
32. Souza MT, Silva MD, Carvalho R. Revisão integrativa: o que é e como fazer. Einstein. 2010;8(1):102-6. DOI: http://dx.doi.org/10.1590/s1679-45082010rw1134
33. Rosa NM, Lima JF, Inoue KC. Conhecimento da equipe de enfermagem sobre neurointensivismo e a influência da educação contínua. Cienc Cuid Saude. 2013;12(1):112-20. DOI: https://doi.org/10.4025/cienccuidsaude.v12i1.15031
34. Uğraş GA, Yüksel S, Temiz Z, Eroğlu S, Şirin K, Turan Y. Effects of Different Head-of-Bed Elevations and Body Positions on Intracranial Pressure and Cerebral Perfusion Pressure in Neurosurgical Patients. J Neurosci Nurs. 2018;50(4):247-51. DOI: https://doi.org/10.1097/JNN.0000000000000386
35. Sacco TL, Delibert SA. Management of intracranial pressure: part I: pharmacologic interventions. Dimens Crit Care Nurs. 2018;37(3):120-9. DOI: https://doi.org/10.1097/DCC.0000000000000293
36. Nyholm L, Steffansson E, Fröjd C, Enblad P. Secondary insults related to nursing interventions in neurointensive care: a descriptive pilot study. J Neurosci Nurs. 2014;46(5):285-91. DOI: https://doi.org/10.1097/JNN.0000000000000077
37. Robinson JD. Management of refractory intracranial pressure. Crit Care Nurs Clin. 2016 [Epub 2015 Nov. 18];28(1):67-75. DOI: https://doi.org/10.1016/j.cnc.2015.09.004
38. Szabo CM, Grap MJ, Munro CL, Starkweather A, Merchant RE. The effect of oral care on intracranial pressure in critically ill adults. J Neurosci Nurs. 2014;46(6):321-9. DOI: https://doi.org/10.1097/JNN.0000000000000092
39. Carney N, Totten AM, O’Reilly C et al. Guidelines for the management of severe traumatic brain injury, Fourth Edition. Neurosurg. 2017;80(1): 6-15. DOI: https://doi.org/10.1227/NEU.0000000000001432
40. Ladanyi S, Elliot D. Traumatic brain injury: An integrated clinical case presentation and literature review Part II: The continuum of care. Aust Crit Care. 2008,21(3):141-53. DOI: https://doi.org/10.1016/j.aucc.2008.02.003
41. Littlejohns L, Bader M. Monitoring technologies in critically ill neuroscience patients. Boston: Jones and Bartlett; 2009.
42. Liontakis IM. No que consiste a monitorização neurológica à beira do leito? Rev Assoc Med Bras. 2005;51(5):243-4. DOI: http://dx.doi.org/10.1590/S0104-42302005000500005
43. Hawthorne C, Piper I. Monitoring of intracranial pressure in patients with traumatic brain injury. Frontiers of Neurology. 2015:121. DOI: https://doi.org/10.3389/fneur.2014.00121
44. Presciutti M. (2006). Nursing priorities in caring for patients with intracerebral hemorrhage. J Neurosci Nurs. 2006 [Epub 2019 Sept. 12];38(4 Suppl):296-9, 315. Available from: https://journals.lww.com/jnnonline/Abstract/2006/09000/Nursing_Priorities_in_Caring_for_Patients_with.5.aspx
45. Jiang Y, Ye Zp, You C, Hu X, Liu Y, Li H, Lin S, Li JP. Systematic review of decreased intracranial pressure with optimal head elevation in post craniotomy patients: a meta-analysis. J Adv Nurs. 2015;71(10):2237-46. DOI: https://doi.org/10.1111/jan.12679
46. Mitchell PH, Kirkness C, Blissitt PA. Chapter 5. Cerebral Perfusion Pressure and Intracranial Pressure in Traumatic Brain Injury. Annu Rev Nurs Res. 2015;33(1):111-83. DOI: https://doi.org/10.1891/0739-6686.33.111
47. Uğraş GA, Aksoy G. The Effects of Open and Closed Endotracheal Suctioning on Intracranial Pressure and Cerebral Perfusion Pressure: A Crossover, Single-Blind Clinical Trial. J Neurosci Nurs. 2012;44(6):E1-8. DOI: https://doi.org/10.1097/JNN.0b013e3182682f69
48. Cerqueira-Neto ML, Moura ÁV, Scola RH, Aquim EE, Rea-Neto Á, Oliveira MC et al. The effect of breath physiotherapeutic maneuvers on cerebral hemodynamics: a clinical trial. Arq. Neuro-Psiquiatr. 2010;68(4):567-72. DOI: http://dx.doi.org/10.1590/S0004-282X2010000400017
49. ChiviteFN, Martnez OA, Marraco BM,Navarro GMA, Nuin ES, Gomez de Segura Nieva JL et al. Intracranial pressure response during secretion aspiration after administration of a muscle relaxant. Enferm Intensiva. 2005 [Epub 2019 Sept. 12];16(4):143-52. Available from: https://www.elsevier.es/es-revista-enfermeria-intensiva-142-articulo-respuesta-presion-intracraneal-durante-aspiracion-13080876
50. Chagas MV, Silva CF, Kinalski SS, Graube SL, Anschau GO, Stumm EMF et al. Assistência ao paciente hospitalizado em UTI: cuidados de enfermagem na aspiração de secreções e circuito ventilatório. RICSB.2018;2(2). DOI: http://dx.doi.org/10.31512/ricsb.v2i2.2774
51. Galbiati G, Paola C. Effects of Open and Closed Endotracheal Suctioning on Intracranial Pressure and Cerebral Perfusion Pressure in Adult Patients with Severe Brain Injury: A Literature Review. J Neurosci Nurs. 2015;47(4):239-46. DOI: https://doi.org/10.1097/JNN.0000000000000146
52. Frota OP, Loureiro MDR, Ferreira AM. Aspiração endotraqueal por sistema aberto: práticas de profissionais de enfermagem em terapia intensiva. Esc Anna Nery. 2014;18(2):296-302. DOI: https://doi.org/10.5935/1414-8145.20140043
53. Barría PRM. Implementing Evidence-Based Practice: A challenge for the nursing practice. Invest Educ Enferm. 2014;32(2):191-3. DOI: https://doi.org/10.17533/udea.iee.v32n2a01
54. Saunders H, Vehviläinen-Julkunen K. Nurses’ Evidence-Based Practice Beliefs and the Role of Evidence-Based Practice Mentors at University Hospitals in Finland. World Views Evid Based Nurs. 2017 [Epub 2018 Dec. 21];14(1):35-45. DOI: https://doi.org/10.1111/wvn.12189
55. Weaver DL, Bradford JL. Neurologic system function, assessment and therapeutic measures. Williams LS, Hooper PD. Understanding Medical Surgical Nursing. 5th edition Philadelphia: F.A. Davis Company; 2015. p. 1095-1210.
56. Cook NF, Deeny P, Thompson K. Management of fluid and hydration in patients with acute subarachnoid hemorrhage: An action research project. Journal of Clinical Nursing. 2004;13(7):835-49. DOI: https://doi.org/10.1111/j.1365-2702.2004.01001.x
57. McNett M. Intensive care unit nurse characteristics impacting judgments about secondary brain injury. Dimens Crit Care Nurs. 2009;28(4):182-8. DOI: https://doi.org/10.1097/DCC.0b013e3181a473d7
58. McNett M, Doheny M, Sedlak C,Ludwick R. Judgments of critical care nurses about risk for secondary brain injury. Am J Crit Care. 2010 [Epub 2009 Jun. 18];19(3):250-60. DOI: https://doi.org/10.4037/ajcc2009293
59. Souza I. O Papel do Enfermeiro Especialista em AVC num Hospital de Londres: Uma Realidade Distante ou Próxima da Portuguesa? Nursing: 2016 [Epub 13 Sept. 2019]. Available from: https://www.nursing.pt/o-papel-do-enfermeiro-especialista-em-avc-num-hospital-de-londres-uma-realidade-distante-ou-proxima-da-portuguesa/
60. Regis LFLV, Porto IS. Basic human needs of nursing professional situations of dissatisfaction at work. Rev Esc Enferm USP. 2011;45(2):332-8. DOI: http://dx.doi.org/10.1590/S0080-62342011000200005
61. Araujo OF, Sousa CLM, Muniz MV, Oliveira AB, Neto NGF, Sousa EPD. Diagnósticos de Enfermagem e Proposta de Intervenções ao paciente com aneurisma cerebral. Com Ciências Saúde. 2014 [Epub 12 Sept. 2019];25(1):25-34. Available from: http://bvsms.saude.gov.br/bvs/periodicos/diagnosticos_enfermagem_proposta.pdf
62. Koizumi MS. Avaliação neurológica utilizando a Escala de Coma de Glasgow: origem e abrangência. Acta Paul Enferm. 2000 [Epub 12 Sept. 2019];13(1):90-4. Available from: https://www2.unifesp.br/acta/index.php?volume=13&numero=1&item=res10.htm