|
Article
Igor Emanuel Soares-Pinto1 ,
Sílvia Maria Moreira Queirós2
Paulo Jorge Pereira Alves3
Tânia Manuel Sousa Carvalho4
Célia Samarina Vilaça de Brito Santos5
Maria Alice Correia de Brito6
1 ![]() 0000-0003-3739-2020 Universidade Católica Portuguesa, Portugal. igor.pinto@ulsm.min-saude.pt
0000-0003-3739-2020 Universidade Católica Portuguesa, Portugal. igor.pinto@ulsm.min-saude.pt
2 ![]() 0000-0002-1884-0134 Universidade Católica Portuguesa, Portugal. silvia.queiros@chsj.min-saude.pt
0000-0002-1884-0134 Universidade Católica Portuguesa, Portugal. silvia.queiros@chsj.min-saude.pt
3 ![]() 0000-0002-6348-3316 Universidade Católica Portuguesa, Portugal. pjalves@porto.ucp.pt
0000-0002-6348-3316 Universidade Católica Portuguesa, Portugal. pjalves@porto.ucp.pt
4 ![]() 0000-0003-0915-9950 Universidade Católica Portuguesa, Portugal. s-tmscarvalho@ucp.pt
0000-0003-0915-9950 Universidade Católica Portuguesa, Portugal. s-tmscarvalho@ucp.pt
5 ![]() 0000-0001-9198-2668 Escola Superior de Enfermagem do Porto, Portugal. celiasantos@esenf.pt
0000-0001-9198-2668 Escola Superior de Enfermagem do Porto, Portugal. celiasantos@esenf.pt
6 ![]() 0000-0003-4414-4383 Escola Superior de Enfermagem do Porto,
Portugal. alice@esenf.pt
0000-0003-4414-4383 Escola Superior de Enfermagem do Porto,
Portugal. alice@esenf.pt
Received: 07/02/2021
Sent to peers: 26/05/2021
Approved by peers: 01/10/2021
Accepted: 04/10/2021
Theme: Chronic care, promotion and prevention.
Contribution to the discipline: Self-care competence in a bowel elimination ostomy is a factor commonly associated to facilitating adaptation to life with a stoma, improving quality of life, and reducing stoma and peristomal skin complications. Nurses play a central and often exclusive role in promoting self-care in people with an ostomy. Several nursing interventions and their direct and indirect outcomes were identified to promote self-care for the bowel elimination ostomy.
Para citar este artículo / To reference this article / Para citar este artigo: Soares-Pinto IE, Queirós S, Alves P, Carvalho T, Santos C, Brito MA. Nursing Interventions to Promote Self-Care in a Candidate for a Bowel Elimination Ostomy: Scoping Review. Aquichan. 2022;22(1):e2212. DOI: https://doi.org/10.5294/aqui.2022.22.1.2
Abstract
Objectives: To identify nursing interventions, their
characteristics, and outcomes for promoting self-care in candidates for a bowel
elimination ostomy.
Materials and
methods: A scoping review
was carried out based on the Joanna Briggs Institute's recommendations. For
this, studies published in Portuguese, English, and Spanish on the Web of
Science, CINAHL, and Scopus databases and without a time limit were selected on
November 9, 2020.
Results: Of 2248 articles identified, 41 were
included in this review. We identified 20 nursing interventions associated with
the self-care of patients with an ostomy; most of
them have gaps in their content, method, and frequency or dosing. More than 30
indicators were identified to assess the impact of nursing interventions;
however, most of them were indirect assessments.
Conclusion: There is scarce evidence regarding the
different aspects that must be involved in nursing interventions for patients
with a stoma. Moreover, there is no standardization in methods, frequency, or
dosing of intervention. It is urgent to define the content, method, and
frequency of nursing interventions necessary to promote self-care in patients
with a bowel elimination ostomy and to use assessment
tools that directly measure stoma self-care competence.
Keywords (Source DeCS): Nursing care; evidence-based practice; self-care; ostomy; patient education as topic.
Resumen
Objetivos: identificar las intervenciones de enfermería, sus características y
resultados para promover el autocuidado en candidatos a estoma de eliminación
intestinal.
Materiales y métodos: se llevó a cabo una revisión de alcance
con base en las recomendaciones del Instituto Joanna Briggs. Para
este fin, se seleccionaron estudios publicados en portugués, inglés y español
en las bases de datos Web of Science, CINAHL y Scopus al 9 de noviembre de 2020.
Resultados: de un total de 2248 artículos identificados, se incluyeron 41 en esta revisión. Se identificaron 20 intervenciones de enfermería asociadas
al autocuidado de pacientes con ostomía; la mayoría
tiene lagunas en su contenido, método y frecuencia o dosis. Se identificaron
más de treinta indicadores para evaluar el impacto de las intervenciones de
enfermería; sin embargo, la mayoría de ellas fueron evaluaciones indirectas.
Conclusión: es escasa la evidencia sobre los
diferentes aspectos que deben considerarse en las intervenciones de enfermería
para pacientes con estoma. Además, no existe una estandarización en los
métodos, la frecuencia o la dosis de intervención. Es urgente definir el
contenido, el método y la frecuencia de las intervenciones de enfermería
necesarias para promover el autocuidado en pacientes con estoma de eliminación
intestinal y utilizar herramientas de evaluación que midan directamente ese
autocuidado.
Palabras clave (Fuente DeCS): Atención de enfermería; práctica clínica basada en la evidencia; autocuidado; estomía; educación del paciente como asunto.
Resumo
Objetivos: identificar as intervenções de enfermagem, suas características e resultados para promover o autocuidado em candidatos à estomia intestinal de eliminação.
Materiais e métodos: foi realizada uma revisão de escopo com base nas
recomendações do Instituto Joanna Briggs. Para isso, foram
selecionados estudos publicados em português, inglês e espanhol nas bases de
dados Web of Science, CINAHL e Scopus de 9 de novembro de 2020.
Resultados: de 2 248 artigos identificados, foram incluídos 41 nesta revisão. Foram identificadas 20 intervenções de enfermagem associadas ao
autocuidado de pacientes com estomia; a maioria tem lacunas em seu conteúdo, método e frequência ou dose. Foram identificados mais de 30 indicadores para avaliar o impacto das
intervenções de enfermagem; contudo, a maioria delas foi avaliação indireta.
Conclusões: é escassa a evidência sobre os diferentes aspectos que devem ser
considerados nas intervenções de enfermagem para pacientes com estomia. Além
disso, não há um padrão nos métodos, na frequência ou na dose de intervenção. É urgente definir
o conteúdo, o método e a frequência das intervenções de enfermagem necessárias
para promover o autocuidado em pacientes com estomia intestinal de eliminação e
utilizar ferramentas de avaliação que meçam diretamente esse autocuidado.
Palavras-chave (Fonte DeCS): Cuidados de enfermagem; prática clínica baseada em evidências; autocuidado; estomia; educação de pacientes como assunto.
Introduction
The word ostomy derives from the Greek "stoma" and means "mouth" or opening, being understood as a surgical communication between an internal organ (intestinal or urinary) and the body surface (1). A bowel elimination ostomy is the exteriorization of a part of the intestine through the abdominal wall as an artificial outlet for feces, constructed from the mucous lining of the intestine (2).
Worldwide, about one million people annually undergo ostomy surgery (3). This number is expected to increase, given that the most likely diagnosis for a bowel elimination ostomy is colorectal cancer (4). Currently, colorectal cancer is the third most common type of cancer worldwide, with more than 1.9 million new cases per year (5), whose incidence is predicted to grow by 60 % as of 2040, with more than 3 million new cases per year (6).
A stoma construction is a life-changing event. While this surgery can have several positive effects, such as reducing symptoms and improving health, it can also adversely affect the person (7) physically, psychologically, socially, and spiritually. It may represent a potential threat to all aspects of the lives of people who must not only learn how to manage stoma care but also incorporate it in their daily lives (7-10) . How this event is experienced is conditioned by several factors, including stoma care competence (1,3,11).
Considering the various factors associated with the acceptance process and its impact on quality of life, literature was identified (12-14) sustaining that a systematic and complete care approach by a nurse from the preoperative phase to follow-up after hospital discharge significantly impacts these factors. In addition, the entire perioper-ative approach improves life quality, reduces health costs (7,15), and has a positive effect on the life of the person with an ostomy (13).
The nurse must give the right information to the right person at the right time to reduce some concerns expressed by the person/patient submitted to ostomy construction, being responsible for recognizing and responding to the educational needs of each one (16). Furthermore, the nurse plays an important supporting role for patients facing changes and their impact. These interventions help the person return to their previous life as soon as possible (7).
In an early stage of the educational process, the goal for the person undergoing a stoma surgery is to develop autonomy and selfcare, increasing their quality of life and achieving competence in all aspects of their self-care (17). Perioperative education is a key component in approaching a person with a stoma; however, evidence is lacking to support improved outcomes. It is crucial to carry out more in-depth studies using rigorous models to design a viable educational intervention that improves patient care and outcomes (15,18).
Implementing intervention programs for the person with a bowel elimination ostomy, considering the different moments of nurse intervention, enhances the management of stoma care, emphasizing adaptation, problem-solving, self-efficacy, cognitive reformulation, and goal definition (19). The present review aims to know the nursing interventions promoting stoma self-care and their characteristics for candidates for a bowel elimination ostomy, from the preoperative phase to follow-up after hospital discharge. It also intends to explore the outcomes used to assess the impact of those interventions.
Materials and methods
A scoping review of the scientific literature was carried out following the methodology of Joanna Briggs Institute (20) and the guidelines established by the PRISMA model (Preferred Reporting Items for Systematic Reviews and Meta-Analyses). For the research structuring and execution, a protocol was developed with information regarding the objectives of this review. The topics are the population to be included in the research, the formulation of the research question, the eligibility criteria, the strategy, and databases used to obtain the relevant information, the definition of topics for data extraction, and how the data would be condensed.
The definition of the starting question followed the strategic parameters P (Population), C (Concept), and C (Context), with the research being guided by the following questions:
• What are the nursing interventions for promoting stoma self-care, from the perioperative period to follow-up after hospital discharge, for a candidate to a bowel elimination ostomy?
• What are the outcomes used to assess nursing interventions to promote bowel elimination ostomy self-care?
Firstly, a preliminary search for possible similar studies was carried out in the CINAHL database in August 2019. Secondly, we conducted another search on the Web of Science, CINAHL Complete, and Scopus databases on September 4, 2019, using combinations based on MeSH, Cinahl Headings, and natural language, as shown in Table 1. Given the time elapsed from research completion to the conclusion of article analysis, new research was carried out on November 9, 2020.
Table 1. Bibliographic research strategies
Web of Science |
CINAHL Complete |
Scopus |
(* stom * NOT tracheostom * NOT cystostom * NOT urostom *) AND ("model of care" OR "care model" OR model * OR "patient * education" OR "centered care" OR discharge *) AND nurs * |
(* stom * NOT tracheostom * NOT cistostom * NOT urostom *) AND ("model of care" OR "care model" OR model * OR "patient * education" OR "centered care" OR discharge *) AND nurs * |
(* stom * AND NOT tracheostom * AND NOT cystostom * AND NOT urostom *) AND ("model of care" OR "care model" OR model * OR "patient * education" OR "centered care" OR discharge *) AND nurs * |
Source: Own elaboration
The selection criteria for the articles were: studies that included people referred to or with a bowel elimination ostomy, either permanent or temporary, aged 18 years or older, and with a potential for regaining autonomy; addressed nursing interventions to promote stoma self-care; in in the preoperative, postoperative, or post-hospital contexts; were primary or secondary studies, qualitative or quantitative, published in Portuguese, English or Spanish, with no time limit.
The research carried out in the databases was loaded and grouped in the ZOTERO 5.0.96.3 software (21), and the duplicates were removed. Two researchers independently conducted the search in databases and the analysis and selection of the articles. In the case of disagreement on the inclusion of any article, a third researcher was consulted.
The title and abstract of the identified studies were evaluated in the first phase based on the pre-established eligibility criteria. Posteriorly, all articles included in the first phase were submitted to the analysis process after full reading. Figure 1 highlights the process of identifying and selecting the articles included in the review.
Figure 1. Search and study selection process - PRISMA Diagram flow
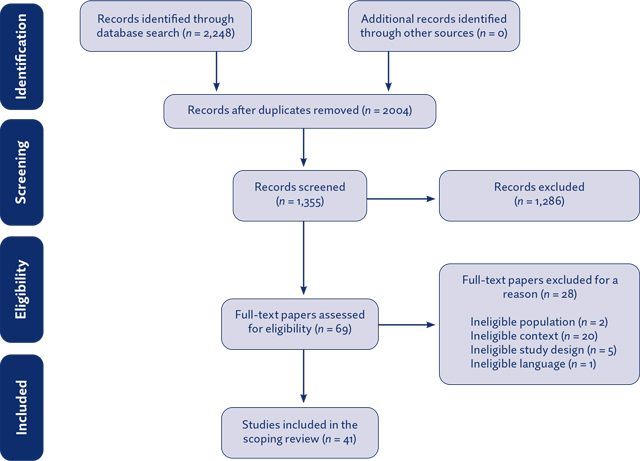
Source: Prisma — Flowchart for scoping review (adapted) (22)
Finally, two independent reviewers extracted data using the data extraction tool developed by the authors for this purpose according to the following aspects: year of publication; country where the research was carried out; objective of the research; type of study; methodological approach; nursing interventions, as well as the content, method, and dosing of interventions. Since this review does not collect deeply personal, sensitive, or conidential information from participants and uses documents accessible to the public as evidence, it does not require approval of an ethics committee.
Results
Of 2248 articles identified, 41 were included in the scoping review, with publication dates from 2004 to 2020: 24 % (10) in 2020, 19.5 % (8) in 2019, 17 °% (7) in 2012, and 12.2 <% (5) in 2018.
Regarding the type of study, the majority are experimental (14) and quasi-experimental studies (6), followed by literature reviews without a defined method (10), systematic literature reviews (3), cohort studies (3), economic analysis (1), and mixed and qualitative studies (4).
The 41 included studies cover a popualtion spread over 13 countries from five different continents: China (5 °%), Thailand (5 °%), Taiwan (7 °%), Singapore (2 °%), Turkey (2 °%), Iran (2 °%), Brazil (2 °%), United States of America (24 °%), United Kingdom (22 °%), Norway (2 °%), Sweden (2 °%), Spain (2 °%), and Australia (2 °%).
All analyzed articles refer to nursing interventions in promoting self-care in a candidate for or a person with a bowel elimination ostomy. Some articles analyze the impact of nursing interventions on different indicators.
Considering the elements that underlie the design of a nursing intervention (22), and to facilitate the reading and analysis of the references included in this review, Table 2 shows the interventions identified, as well as the content, method of administration, and dosing of each intervention, including amount, frequency, and duration. The syntax of interventions was adjusted to the Classification of Interventions for Nursing Practice (CIPE), version 2019, as it is an international language used to document nursing care.
Table 2. Nursing interventions to promote stoma self-care in a candidate for a bowel elimination ostomy
Intervention |
Time |
Content |
Method |
Dosing (quantity / frequency /duration) and moment |
Preoperative |
Justifying and explaining to the user the choice of the stoma site (16, 26) |
One session (26) On the day of admission to the hospital (23, 28) |
||
Encouraging the manipulation of ostomy devices (25) |
Preoperative |
-— |
-— |
-— |
Promoting interaction with people with a bowel elimination ostomy (25) |
Preoperative |
-— |
-— |
-— |
Assessing the potential for stoma self-care (29) |
Postoperative -hospitalization |
Assessing the presence of co-morbidities or psychomotor deficits that condition the capacity for self-care (arthritis, paralysis, fatigue, visual problems) (29) |
||
Preoperative |
Information about
nurses who follow up from the preoperative period until after hospital
discharge (16, 27) |
Face to face (27) |
Two sessions (28) A session on the day of admission (28) |
|
Postoperative -hospitalization |
Providing support
contacts (30, 31, 35) |
Face to face (30) |
At discharge (31) |
|
After hospital discharge |
Informing about
available resources (25, 32): |
—- |
||
Teaching about bowel elimination ostomy (16, 23- 28, 30, 31, 36 -41) |
Preoperative |
Teaching about
the stoma formation process (10, 23, 25, 28, 30, 31): |
Face to face -
home (23) |
Two sessions (23, 28), which can be at home (23) |
Postoperative -hospitalization |
Teaching about
the stoma formation process (10, 24, 25, 40): |
Face to face (40) |
One session (27) |
|
Teaching bowel elimination ostomy self-care (7,16,23,25,27-29,31 -33, 35,40-51) |
Preoperative |
Showing ostomy devices indicated for the stoma (16, 23, 28) |
Face to face (24, 41): |
Two sessions (23) |
Postoperative -hospitalization |
Defining goals to
be achieved with the user (16) |
Face to face (27,
31, 40, 42, 44, 47) |
Starting as soon
as possible after surgery (23, 37, 42), even on the day of
surgery (37) or the first postoperative day (16, 28, 40, 47) |
|
After hospital discharge |
Addressing device
removal and application procedure (32, 33, 46) |
Face to face (27, 46) |
Once a month (7, 46) for six months (7) |
|
Teaching about bowel elimination ostomy complications (7, 25, 29, 31, 32, 35, 41, 42, 45, 46, 51) |
Preoperative |
Teaching about
complications: |
Face to face (25): |
|
Postoperative -hospitalization |
- Stoma and skin
assessment (10, 42) |
Face to face (42) Use of digital media - DVD / video (45) |
Starting as early as possible after surgery(42) |
|
After hospital discharge |
- Risk of
dehydration (25) |
Face to face (25) |
Once a month for six months after discharge (7) |
|
Preoperative |
Demonstration of application, emptying, and how to change the effluent collection device, one or two pieces according to the type of stoma (23- 26, 28, 36) |
Face to face (23- 26, 36) |
Two sessions (28) at home (23) |
|
Instructing on bowel elimination ostomy self-care (24- 26, 28, 31, 36, 40, 41, 45, 50, 53) |
Postoperative -hospitalization |
Procedure for
removal, hygiene, and application of the device (50) |
Face to face (30, 42) |
Starting as early
as possible after surgery (42), e.g., first postoperative day (30) |
After hospital discharge |
Face to face (53) |
The first month
after discharge |
||
Assessing stoma self-care competence (7, 25, 27, 33, 44, 46, 51, 53- 55) |
Preoperative |
Changing the ostomy device (23) |
Use of a model (23) |
In the second session of two, at home (23) |
Postoperative -hospitalization |
Eighteen topics considered minimal aspects for discharge, centered on knowledge and performance of stoma self-care, stoma and skin self-surveillance, and resource management (55) |
At discharge (55) |
||
After hospital discharge |
Parameters of the self-care agency scale (ESCA) (44) |
Telephone contact
(7, 44, 51, 53, 54, 56, 57) |
Sessions according to the needs of the user or family (25) |
|
Training bowel elimination ostomy self-care (25, 27, 30, 41- 43, 45, 47, 59) |
Postoperative -hospitalization |
Removal, hygiene,
and cleaning procedure (50) |
Face to face (23) Use of an ostomy simulator (50) |
Starting on the 1st postoperative day and scheduling remaining training based on the user's needs (30) All possible opportunities (42) In the 2nd and third training sessions (45) Four sessions (50) 40 minutes (47) |
After hospital discharge |
Focused on
problem-solving: |
Face to face Group sessions managed by a nurse (59) |
||
Planning follow-up consultation after hospital discharge (7, 23, 27, 31, 34, 41, 43, 44, 46, 52, 58) |
Postoperative – hospitalization |
Informing about follow-up contacts: |
Face to face (23, 25, 31) |
One hour (41) |
After hospital discharge |
Focused on
problem solving: |
Face to face Group sessions managed by a nurse (59) |
One-hour sessions (59) |
|
Assessing for signs of stoma and peristomal skin complications (7, 16, 25, 27, 31, 44, 46) |
Postoperative -hospitalization |
Skin evaluation with Ostomy Skin Tool (16) |
—- |
------- |
After hospital discharge |
Hemorrhage, stenosis, allergic dermatitis, edema, and mucocutaneous dehiscence (44) |
Face to face (44) |
Once a week for four to five months (44, 46) or six months (7) |
|
After hospital discharge |
Persuasion for
stoma self-care (32) |
------- |
------- |
|
Assessing knowledge of stoma and peristomal skin complications (25, 27) |
After hospital discharge |
------- |
------- |
------- |
After hospital discharge |
------- |
Telephone contact (46) |
------- |
|
After hospital discharge |
------- |
------- |
------- |
|
Evaluating the use of health resources (56) |
After hospital discharge |
------- |
------- |
------- |
Informing about health resources (31) |
After hospital discharge |
------- |
------- |
------- |
Teaching about self-surveillance (33) |
After hospital discharge |
Verifying changes and solutions used for troubleshooting (33) |
Face to face (33) |
------- |
Source: Own elaboration
We could identify 20 nursing interventions associated with the self-care of the patient with an ostomy. Those interventions are described at various times (pre- and immediate postoperative period, during hospitalization, and even after hospital discharge). We also found adequate interventions only at one point in the hospitaliza-tion period (pre- and post-hospitalization or discharge) or interventions performed at various times, with the following distribution: four interventions during the preoperative period, five interventions during postoperative inpatient, and 16 interventions after hospital discharge.
As for the implementation methods used, most contact is face-to-face (77 %), in the hospital (67 %), or at home (33 %). Other options are contact by telephone (10 °%) or through a smartphone application (13 %%).
The used resources in most interventions are in writing, with the most referenced information being in a leaflet format. Digital support is also employed, namely videos, photographs, or 2D animations. For teaching, instructing, and training interventions, simulators or models are a common approach.
In the analysis of the included articles, we identified indicators to assess the impact of one or more interventions. Table 3 shows the outcomes and the method used for their assessment —answering the second research question—, the outcomes of the nursing interventions for the promotion of stoma self-care, and the instruments used to assess these results.
Table 3.Outcomes and methods for assessing the impact of nursing interventions
Outcomes |
Assessment method |
General readmission rate; readmission rate for dehydration (28, 51) or kidney failure (51); readmission rate for complications associated with the ostomy (39); readmission rate up to 30 days after discharge (51) |
|
Number of consultations / contacts with health professionals (23, 53), including unplanned ones (48) |
|
Time of contact with a nurse (7) |
|
Use of hospital consumables (7) |
|
Estimated direct costs (51) |
30 days after surgery (51) |
Incidence of early complications (28) |
|
Form to assess Ostomy Complication (43, 44) or Ostomy Complication Severity Index (OCSI) (7) |
|
Health-related quality of life (28) |
HRQoL - Generic 15D instrument (28) |
Sleep quality,
activity, mental state, and appetite (43) |
|
Quality of life associated with adaptation to an ostomy (27) |
Questionnaire to assess physical, psychological, and social adaptation to an ostomy (27) |
Major and minor morbidities (28) |
|
Self-rating Anxiety Scale (SAS) (43, 46) |
|
State-Trait Anxiety Inventory (STAI) (33) |
|
Depression (23) |
|
The self-designed disease knowledge questionnaire (includes complication management, knowledge of drug use, device change) (46) |
|
Knowledge of the ostomy (43) |
|
Knowledge of, attitude, and behavior towards ostomy self-care (40) |
Behavior Assessment Form (Behavior Skills) (47) |
Psychological adaptation (31) |
|
Ostomy Adjustment Scale (54), Ostomy Adjustment Inventory (OAI) (7), Ostomy Adjustment Inventory-23 (OAI-23) (50) |
|
Self-efficacy scale (31), Stoma Self-efficacy Scale (33, 50, 54) |
|
Confidence for self-care (45) |
Visual Analog Scale (EVA) (45) |
Ostomy self-management (41) |
Questionnaire Form for Self-management of Ostomy (41) |
Number of days / weeks until autonomy in self-care (23, 48, 53) |
|
Degree of user satisfaction (23, 33, 44, 46, 49, 51, 53, 54) |
|
Questionnaire on areas of intervention and level of satisfaction (very satisfied, satisfied, dissatisfied) (43) |
|
User perception regarding the usefulness of the nurse's intervention (56) |
|
Intervention effectiveness rate (26) |
|
Evaluation of the quality of multimedia resources (49) |
Source: Own elaboration
We established a relationship between interventions and indicators since this information is not expressed objectively in the literature. In addition, the same indicator can respond to a single or all interventions.
Discussion
This paper is the first literature review to map nursing interventions centered on promoting the self-care of a candidate for or a person with a bowel elimination ostomy. The review showed that research is conducted within the scope of the definition of nursing interventions prescribed to the candidate or person with a bowel elimination ostomy, noting that most are experimental studies. However, those are more directed towards assessing methods for implementing nursing interventions, namely simulators (50), telephone contact (43, 54), mobile apps (31), and multimedia resources (40).
Methods to improve the educational process of patients through information and communication technologies, such as computer-aided education models, are evolving rapidly, and nurses play a central and privileged role in using these technologies to enhance and optimize their interventions for patients (49). The technology most referred to in the literature is a communication-only mobile phone application. However, technology, especially mobile technology, is being used by community nurses for various purposes, including knowledge sharing, reporting, and caseload planning (60). Advances in information technologies, such as smartphones and mobile applications, have created more opportunities for people to have information related to their health status available at any time or place according to their needs and preference.
As health professionals with exclusive intervention in promoting stoma self-care, nurses must develop content that integrates into different implementation methods, whether using mobile phone applications, videos, or interactive images. This content is the disciplinary knowledge of nursing.
For the challenges faced by health professionals and people with an ostomy regarding reduced hospitalization time and increased complex therapy, whether surgical or pharmacological, it is pertinent to develop instruments that facilitate and enhance the acquisition of stoma self-care competence. The literature maintains that self-care competence positively influences the adaptation process to the stoma (54) and life quality (28, 43), reduces the incidence of stoma and peristomal skin complications (43, 44), and increases self-efficacy (44) and confidence in self-care (45). It is also evident that the most significant difficulties experienced after discharge are related to insufficient knowledge and the capacity for self-care and pre- and postoperative care (10). The results promote the importance of the nurse's intervention in the three perioperative moments to develop the stoma self-care competence.
The designed nursing interventions presume the definition of the content, the method of administering it, and the dosing, which includes the intervention's frequency, duration, and intensity (22, 61). However, no studies addressing these characteristics systematically and completely were identified. From the identified literature, specific interventions are mentioned without any reference to content, method, and dosing, namely "Encouraging the manipulation of ostomy devices," "Promoting interaction with people with a bowel elimination ostomy," "Assessing knowledge of stoma and peristomal skin complications," "Assessing the diet," "Assessing intestinal elimination," "Assessing the use of health resources" and "Informing about health resources."
The content is the most described component in the remaining interventions and where there is the most significant consensus. Meanwhile, the administration method and dosing are referenced but is incomplete in most articles, with the dosing being the component of interventions with major discrepancies and less information available.
Within each intervention, we identified that they are repeated throughout the different administration moments (preoperative phase, postoperative hospitalization, or after hospital discharge). However, there are differences in the content and dosing of interventions at each moment.
In the preoperative period, concerning the method for the different interventions, these can be in person, via telephone, or both, the most common being only one face-to-face session on the eve of the surgery (24, 26, 36- 39). Regardless of the interventions, method, and dosing, it is agreed that when performed preoperatively, they significantly impact the well-being of the person with a stoma, the reduction of complications, and the use of health resources (62, 63). In addition, there seems to be a consensus among all authors on performing stoma site and the positive impact it has (62). In this context, "teaching about intestinal elimination ostomy" and "teaching about bowel elimination ostomy self-care" appear to be the most referenced preoperative interventions in the literature.
Concerning the interventions implemented in the postoperative period, during hospitalization, we found comparative studies between the use of the face-to-face expository method, face-to-face intervention combined with multimedia resources, or the exclusive use of multimedia methods. The results suggest that the use of multimedia tools can be used to implement the intervention. Nevertheless, it is enhanced when combined with the face-to-face intervention by the nurse (40, 45). One aspect to be considered before the execution of any nursing intervention to promote self-care is to ensure that the patient is prepared and available without any discomfort or pain (42). The use of the internet has emerged as an intervention method with excellent cost-effectiveness in the following cases: "Teaching about bowel elimination ostomy," and "Teaching about bowel elimination ostomy self-care," (31, 64).
Considering the approach after hospital discharge, the methods of implementing the interventions are telephone or face-to-face contact in the context of a consultation in a hospital or through home visits. Telephone contact emerges as an effective strategy in specific interventions such as "Assessing stoma self-care competence" and "Watching for signs of stoma and peristomal skin complications." These interventions have beneits regarding associated costs and health gains, scope of customer satisfaction, improved adaptation to the stoma, perception of self-efficacy, and reduced incidence of stoma or peristomal skin complications (54, 56).
Consensus among the authors was identified regarding follow-up by a stoma nurse and early start of follow-up, namely in the first week after hospital discharge, being the non-face-to-face contact via telephone call one of the most mentioned methods (54, 56, 65).
The intervention "Planning a follow-up appointment after hospital discharge" is the one with more variable dosing options after discharge. However, the first six weeks are defined as the most vulnerable phase and require a closer intervention (25, 27, 44).
Some studies evaluated the impact that interventions, or a set of them, could have on specific indicators. From the analysis of Table 2, not all authors express how they evaluate the indicator in question, which emerges as a limitation to research rigor and replication. In the review context, the indicators most sensitive to nursing interventions are highlighted, which we group into ive categories: safety, economic, psychological well-being, functional status and, symptom experience (22).
In the sensitive results to nursing interventions and safety categories, the incidence of stoma and peristomal skin complications was considered, which stands out as the most common in the articles, followed by economic results as length of stay, the rate of hospital readmission, and the number of consultations.
For the psychological well-being category, indicators such as anxiety, depression, and negative emotions are used. The functional status category groups indicators such as adaptation and the capacity for self-care and indirect indicators such as user satisfaction. For the symptom experience category, no indicator is shown.
Considering the direct and autonomous intervention of nurses in promoting stoma self-care, they would be expected to use reliable and rigorous instruments to assess the level of stoma self-care competence (66). However, only three authors use direct indicators to assess the impact of nursing interventions on self-care competence (41, 44, 46), while the remaining indicators evaluate it indirectly. For assessing the impact of interventions, their contents, methods, and dosing on self-care competence, it is imperative to use direct indicators, that is, stoma self-care competence of and the dimensions comprising it (66).
Regarding the analyzed literature, the interventions and the contents to be included in the different moments of the perioperative period are defined; nevertheless, they are still poorly consolidated. It should be noted that the period after hospital discharge is the one that lacks the most evidence regarding the definition of nursing interventions, contents, and dosing, also emerging as the period of greatest vulnerability for the person with a new ostomy (67).
This review highlights evidence that can facilitate the intervention of nurses in providing care to the person proposed for stoma construction or after its construction. The results of this review must be examined in light of several limitations. The broad nature of our Boolean research phrase was intended to include the most significant number of studies, but did not cover all the databases and gray literature, certainly excluding some references.
Conclusion
Stoma self-care is enhanced by an appropriate nursing intervention from the preoperative moment, to the immediate postoperative period, to adjusted follow-up after hospital discharge. The promotion of self-care is a critical component in the recovery of people with an ostomy, with a significant impact on several indicators sensitive to the intervention of nurses, namely functional status, safety, and psychological and economic impact. The knowledge and use of these indicators are of crucial importance for, on the one hand, highlighting the condition of patients, and on the other hand, demonstrating the relevance of nursing care to the person.
While there is available literature that supports the nurse's intervention in elimination ostomy self-care, more research is needed on the definition of content, methods, and dosing of interventions, especially after hospital discharge where a more significant lack of information and vulnerability of the person with a new ostomy are detected.
There is no evidence to support the improvement in clinical results, suggesting that further studies should be carried out through rigorous programs to develop a viable educational intervention that improves the care provided to patients.
The use of multiple and indirect outcomes in assessing nursing interventions is beneficial to understand their impact on different areas; however, a direct indicator of the objective of the intervention should always be used. Thus, when evaluating interventions or intervention programs aimed at promoting stoma self-care, it is crucial to employ tools that directly assess self-care competence.
Conflicts of interest: None declared.
References
1. Giordano V, Nicolotti M, Corvese F, Vellone E, Alvaro R, Villa G. Describing self-care and its associated variables in ostomy patients. J Adv Nurs [Internet]. 2020 [cited 2020 Nov 29];76(11):2982-2992. DOI: https://doi.org/10.1111/jan.14499
2. Di Gesaro A. Self-care and patient empowerment in stoma management. Gastrointest Nurs [Internet]. 2012;10(2):19-23. DOI: https://doi.org/10.12968/gasn.2012.10.2.19
3. Simmons KL, Smith JA, Bobb K-A, Liles LLM. Adjustment to colostomy: Stoma acceptance, stoma care self-efficacy and interpersonal relationships. J Adv Nurs[Internet]. 2007;60(6)627-635. DOI: https://doi.org/10.4314/ejhs.v26i2.5
4. Engida A, Ayelign T, Mahteme B, Aida T, Abreham B. Types and Indications of Colostomy and Determinants of Outcomes of Patients After Surgery. Ethiop J Health Sci [Internet]. 2016 [cited 2020 Mar 10];26(2):117-120. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4864340/
5. International agency for research on cancer. Cancer today [Internet]; 2021 [cited 2021 Sep 29]. Available from: http://gco.iarc.fr/today/home
6. International agency for research on cancer. Cancer Tomorrow [Internet]; 2021 [cited 2021 Sep 29]. Available from: https://gco.iarc.fr/tomorrow/en/dataviz/bars?mode=cancer&populations=900&-cancers=9_8&group_cancers=1&multiple_cancers=1&multiple_populations=0
7. Cengiz B, Bahar Z, Canda AE. The Effects of Patient Care Results of Applied Nursing Intervention to Individuals With Stoma According to the Health Belief Model. Cancer Nurs [Internet]. 2020;43(2):E87~E96. DOI: https://doi.org/10.1097/NCC.0000000000000678
8. Sousa CF, Santos C, Graça LCC. Construção e validação de uma escala de adaptação a ostomia de eliminação. Rev Enfermagem Referência [Internet]. 2015;serIV(4):21-30. DOI: https://doi.org/10.12707/RIV14021
9. Byfield D. The Lived Experiences of Persons With Ostomies Attending a Support Group A Qualitative Study. J Wound Ostomy-Continence Nurs [Internet]. 202047(5)489-495. DOI: https://doi.org/10.1097/WON.0000000000000696
10. de Sena JF, da Silva IP, Lucena SKP, Oliveira ACS, Costa IKF. Validation of educational material for the care of people with intestinal stoma. Rev Lat Am Enfermagem [Internet]. 2020;28:1-9. DOI: https://doi.org/10.1590/1518-8345.3179.3269
11. Elshatarat RA, Ebeid IA, Elhenawy KA, Saleh ZT, Raddaha AHA, Aljohani MS. Jordanian ostomates' health problems and self-care ability to manage their intestinal ostomy: a cross-sectional study. J Res Nurs [Internet]. 2020 [2020 Nov 29];1744987120941568. DOI: https://doi.org/10.1177/1744987120941568
12. Colwell JC, Gray M. Does preoperative teaching and stoma site marking affect surgical outcomes in patients undergoing ostomy surgery? J Wound Ostomy Continence Nurs [Internet]. 2007;34(5):492-496. DOI: https://doi.org/10.1097/01.WON.0000290726.08323.a6
13. Millan M, Tegido M, Biondo S, García-Granero E. Preoperative stoma siting and education by stomatherapists of colorectal cancer patients: a descriptive study in twelve Spanish colorectal surgical units. Colorectal Dis [Internet]. 2010;12(7):e88-e92. DOI: https://doi.org/10.1111/j.1463-1318.2009.01942.x
14. Person B, Ifargan R, Lachter J, Duek SD, Kluger Y, Assalia A. The impact of preoperative stoma site marking on the incidence of complications, quality of life, and patient's independence. Dis Colon Rectum [Internet]. 2012;55(7)783-787. DOI: https://doi.org/10.1097/DCR.0b013e31825763f0
15. Danielsen AK, Burcharth J, Rosenberg J. Patient education has a positive effect in patients with a stoma: a systematic review. Colorectal Dis [Internet]. 2013;15(6):276-283. DOI: https://doi. org/10.1111/codi.12197
16. Bird A, Wilson K, Bertinara A, Amos L. Educating patients in stoma care. Br J Nurs [Internet]. 2019;28(5):S4~S5. DOI: https://doi.org/10.12968/bjon.2019.28.5.S4
17. Krouse RS, Grant M, McCorkle R, Wendel CS, Cobb MD, Tallman NJ, et al. A chronic care ostomy self-management program for cancer survivors. Psycho-Oncology [Internet]. 2016;25(5):574-581. DOI: https://doi.org/10.1002/pon.4078
18. Phatak UR, Li LT, Karanjawala B, Chang GJ, Kao LS. Systematic review of educational interventions for ostomates. Dis Colon Rectum [Internet]. 2014;57(4)529-537. DOI: https://doi.org/10.1097/DCR.0000000000000044
19. Ercolano E, Grant M, McCorkle R, Tallman NJ, Cobb MD, Wendel C, et al. Applying the chronic care model to support ostomy self-management: Implications for oncology nursing practice. Clin J Oncol Nurs [Internet]. 2016;20(3):269-274. DOI: https://doi.org/10.1188/16.CJON.20-03AP
20. Peters M, Godfrey C, McInerney P, Soares C, Hanan K, Parker D. The Joanna Briggs Institute Reviewers' Manual 2015: Methodology for JBI Scoping Reviews; 2015 [2017 Jan 4]. Available from: http://espace.library.uq.edu.au/view/UQ:371443
21. Corporation for Digital Scholarship. Zotero [Internet]; 2020 [cited 2021 Sep 29]. Available from: https://www.zotero.org/
22. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med [Internet]. 2018 [2021 Aug 14;169(7)467-473. DOI: https://doi.org/10.7326/M18-0850
23. Aranda S. Designing nursing interventions. Collegian (Royal College of Nursing, Australia). 2008;1500:19-25. DOI: https://doi.org/10.1016/j.colegn.2007.11.002
24. Chaudhri S, Brown L, Hassan I, Horgan AF. Preoperative intensive, community-based vs. traditional stoma education: a randomized, controlled trial. Dis Colon Rectum [Internet]. 200548(3)504-509. DOI: https://doi.org/10.1007/s10350-004-0897-0
25. Goldberg M, Aukett LK, Carmel J, Fellows J, Folkedahl B, Pittman J. Management of the patient with a fecal ostomy: Best practice guideline for clinicians. J Wound Ostomy Continence Nurs [Internet]. 201037(6)596-598. DOI: https://doi.org/10.1097/WON.0b013e3181f97e37
26. Miller D, Pearsall E, Johnston D, Frecea M, McKenzie M. Executive Summary: Enhanced Recovery After Surgery: Best Practice Guideline for Care of Patients with a Fecal Diversion. J Wound Ostomy Continence Nurs [Internet]. 201744(1)74-77. DOI: https://doi.org/10.1097/WON.0000000000000297
27. Zimnicki KM. Preoperative teaching and stoma marking in an inpatient population: A quality improvement process using a FOCUS-plan-do-check-act model. J Wound Ostomy Continence Nurs [Internet]. 2015;42(2):165-169. DOI: https://doi.org/10.1097/WON.0000000000000111
28. Fingren J, Lindholm E, Petersen C, Hallén A-M, Carlsson E. A Prospective, Explorative Study to Assess Adjustment 1 Year After Ostomy Surgery Among Swedish Patients. Ostomy Wound Manage [Internet]. 2018;64(6):12-22. DOI: https://doi.org/10.25270/owm.2018.6.1222
29. Forsmo HM, Pfeffer F, Rasdal A, Sintonen H, Kórner H, Erichsen C. Pre- and postoperative stoma education and guidance within an enhanced recovery after surgery (ERAS) programme reduces length of hospital stay in colorectal surgery. Int J Surg [Internet]. 2016 [cited 2019 Sep 22];36:121-126. DOI: https://doi.org/10.1016/j.ijsu.2016.10.031
30. Linda B-H, Elliott B. COLOSTOMY CARE A Guide for Home Care Clinicians. Home Healthc Now [Internet]. 20i9;37(2):68-78. DOI: https://doi.org/10.1097/NHH.0000000000000735
31. Adams K. Helping older patients to adapt to stomas using an enhanced recovery programme. Br J Community Nurs [Internet]. 2019;24(5):224-228. DOI: https://doi.org/10.12968/bjcn.2019.24.5.224
32. Wang Q,Wang J, Zhao J, Huo X, Wu L, Yang L, et al. Effects of a home care mobile app on the outcomes of discharged patients with a stoma: A randomised controlled trial. J Clin Nurs [Internet]. 2018;27(19/20):3592-3602. DOI: https://doi.org/10.1111/jocn.14515
33. Zhang J-E, Wong FKY, You LM, Zheng MC. A qualitative study exploring the nurse telephone follow-up of patients returning home with a colostomy. J Clin Nurs [Internet]. 2012;21(9-10):1407-1415. DOI: https://doi.org/10.1111/j.1365-2702.2011.03824.x
34. Xia L. The Effects of Continuous Care Model of Information-Based Hospital-Family Integration on Colostomy Patients: A Randomized Controlled Trial. J Cancer Educ [Internet]. 2020;35(2):301-311. DOI: https://doi.org/10.1007/s13187-018-1465-y
35. Schluter JE, Sinasac PA. Community stomal therapy services: a needs analysis and development of an evidence based model of care. J Stomal Ther Aust [Internet]. 2020 [2020 Nov 9];40(1):8-13. DOI: https://doi.org/10.33235/jsta.40.1.8-13
36. Berti-Hearn L, Elliott B. Ileostomy Care: A Guide for Home Care Clinicians. Home Healthc Now [Internet]. 2019;37(3):136-144. DOI: https://doi.org/10.1097/NHH.0000000000000776
37. Cronin E. What the patient needs to know before stoma siting: an overview. Br J Nurs. 2012;21(22):1304-1308. DOI: https://doi.org/10.12968/bjon.2012.21.22.1234
38. Burch J, Slater R. Enhanced recovery after surgery: benefits for the stoma care patient. Br J Nurs [Internet]. 2012;21(6):S16-21. DOI: https://doi.org/10.12968/bjon.2012.21.Sup6.S16
39. Kittinouvarat S, Charoenlar S, Aeksiriwaranon W. Development of a self-care empowerment model for patients with faecal diversion. WCET J. 2011;31(2):9-14.
40. Nagle D, Pare T, Keenan E, Marcet K, Tizio S, Poylin V. Ileostomy pathway virtually eliminates readmissions for dehydration in new ostomates. Dis Colon Rectum [Internet]. 2012;55(12):1266-1272. DOI: https://doi.org/10.1097/DCR.0b013e31827080c1
41. Lo S-F, Wang Y-T, Wu L-Y, Hsu M-T, Chang SC, Hayter M. Multimedia education programme for patients with a stoma: Effectiveness evaluation. J Adv Nurs [Internet]. 2011;67(1):68-76. DOI: https://doi.org/10.1111/j.1365-2648.2010.05455.x
42. Wen S-L, Li J, Wang A-N, Lv M-M, Li H-Y, Lu Y-F, et al. Effects of transtheoretical model-based intervention on the self-management of patients with an ostomy: A randomised controlled trial. J Clin Nurs [Internet]. 2019;28(9-10):1936-1951. DOI: https://doi.org/10.1111/jocn.14731
43. Kirkland-Kyhn H, Martin S, Zaratkiewicz S, Whitmore M, Young HM. Ostomy Care at Home. Am J Nurs [Internet]. 2018;118(4):63-68. DOI: https://doi.org/10.1097/01.NAJ.0000532079.49501.ce
44. Geng W, Tao N, Wang T, Zhang Y, Wang Y. Continuous nursing reduces postoperative complications and improves quality of life of patients after enterostomies. Int J Clin Exp Med. 2019;12(5):5895-5901.
45. Huang L, Yu H, Sun A, Xu F, Xia C, Gao D, et al. Effects of continuing nursing on stomal complications, self-care ability and life quality after Miles' operation for colorectal carcinoma. Int J Clin Exp Med. 2018;11(2):1021-1026.
46. Crawford D, Texter T, Hurt K, Van Aelst R, Glaza L, Vander Laan KJ. Traditional nurse instruction versus 2 session nurse instruction plus DVD for teaching ostomy care: a multisite randomized controlled trial. J Wound Ostomy Continence Nurs [Internet]. 2012;39(5):529-537. DOI: https://doi.org/10.1097/WON.0b013e-3182659ca3
47. Hu H, Zheng J, Gao L. The effect of continuing nursing services on colostomy patients. Int J Clin Exp Med [Internet]. 2020;13(8):5876-5884. Available from: http://ijcem.com/files/ijcem0114204.pdf
48. Yilmazer T, Tuzer H, Akyüz S. Effect of Information-Motivation-Behavioral Skills Model-Based Intervention on Quality of Life of Ostomy Patients. Turk Klin Hemsire Bilim [Internet]. 2020 [cited 2020 Nov 9];12(2):182-189. DOI: https://doi.org/10.5336/nurses.2019-72070
49. Millard R, Cooper D, Boyle MJ. Improving Self-Care Outcomes in Ostomy Patients via Education and Standardized Discharge Criteria. Home Healthc Now [Internet]. 2020;38(1):16-23. DOI: https://doi.org/10.1097/NHH.0000000000000816
50. Farahani MA, Dorri S, Yousefi F. Design and Validation of Education Multimedia Program for Patients with Fecal Diversions A Quality Improvement Project to Enhance Self-Care. J Wound Ostomy Continence Nurs [Internet]. 2020;47(1):39-44. DOI: https://doi.org/10.1097/WON.0000000000000603
51. Pouresmail Z, Nabavi FH, Abdollahi A, Shakeri MT, Saki A. Effect of using a simulation device for ostomy self-care teaching in Iran: A pilot, randomized clinical trial. Wound Manag Prev [Internet]. 2019;65(6):30-39. DOI: https://doi.org/10.25270/wmp.2019.6.3039
52. Grahn SW, Lowry AC, Osborne MC, Melton GB, Gaertner WB, Vogler SA, et al. System-Wide Improvement for Transitions After Ileostomy Surgery: Can Intensive Monitoring of Protocol Compliance Decrease Readmissions? A Randomized Trial. Dis Colon Rectum [Internet]. 2019;62(3):363-370. DOI: https://doi.org/10.1097/DCR.0000000000001286
53. Marsden J. Enhanced recovery after surgery (ERAS): A literature review of implications for ostomates and stoma care nurses. Gastrointest Nurs [Internet]. 2020;18(1):32-37. DOI: https://doi.org/10.12968/gasn.2020.18.1.32
54. Bohnenkamp SK, McDonald P, Lopez AM, Krupinski E, Blackett A. Traditional versus telenursing outpatient management of patients with cancer with new ostomies. Oncol Nurs Forum [Internet]. 2004;31(5):1005-1010. DOI: https://doi.org/10.1188/04.ONF.1005-1010
55. Zhang J-E, Wong FKY, You L-M, Zheng M-C, Li Q, Zhang B-Y, et al. Effects of enterostomal nurse telephone follow-up on postoperative adjustment of discharged colostomy patients. Cancer Nurs [Internet]. 2013;36(6):419-428. DOI: https://doi.org/10.1097/NCC.0b013e31826fc8eb
56. Colwell JC, Kupsick PT, McNichol LL. Outcome criteria for discharging the patient with a new ostomy from home health care a WOCN society consensus conference. J Wound Ostomy Continence Nurs [Internet]. 2016;43(3):269-273. DOI: https://doi.org/10.1097/WON.0000000000000230
57. Burch J. Enhanced recovery and nurse-led telephone follow-up post surgery. Br J Nurs [Internet]. 2012;21(16):S24--29. DOI: https://doi.org/10.12968/bjon.2012.21.Sup16.S24
58. Quintana J, Catalina Pastor Juan, Prados Herrero I, Pérez López C, González Fuentes M, de Mena Casaseca C, et al. A prospective, longitudinal, multicenter, cohort quality-of-life evaluation of an intensive follow-up program for patients with a stoma. Ostomy/Wound Manag. 2010;56(5):44-52.
59. Johnson T. Follow-up care of stoma patients: a systematic literature review. Gastrointest Nurs [Internet]. 2012;10(9)30-36. DOI: https://doi.org/10.12968/gasn.2012.10.9.30
60. Hornbrook MC, Cobb MD, Tallman NJ, Colwell J, McCorkle R, Ercolano E, et al. Costs of an ostomy self-management training program for cancer survivors. Psycho-Oncology [Internet]. 2018;27(3):879-885. DOI: https://doi.org/10.1002/pon.4584
61. Dewsbury G. Use of information and communication technology in nursing services. Br J Community Nurs [Internet]. 2019;24(12):604-607. DOI: https://doi.org/10.12968/bjcn.2019.24.12.604
62. Conn VS, Rantz MJ, Wipke-Tevis DD, Maas ML. Designing effective nursing interventions. Res Nurs Health. 2001;24(5)433-442. DOI: https://doi.org/10.1002/nur.1043
63. Salvadalena G, Hendren S, McKenna L, Muldoon R, Netsch D, Paquette I, et al. WOCN Society and ASCRS Position Statement on Preoperative Stoma Site Marking for Patients Undergoing Colostomy or Ileostomy Surgery. J Wound Ostomy Continence Nurs [Internet]. 2015;42(3): 249-252. DOI: https://doi.org/10.1097/WON.0000000000000119
64. Wasserman MA, McGee MF. Preoperative Considerations for the Ostomate. Clin Colon Rectal Surg [Internet]. 2017;30(3):157-161. DOI: https://doi.org/10.1055/s-0037-1598155
65. Pittman J, Nichols T, Rawl SM. Evaluation of web-based ostomy patient support resources. J Wound Ostomy Continence Nurs [Internet]. 2017;44(6):550-556. DOI: https://doi.org/10.1097/WON.0000000000000371
66. Lim SH, Chan, SW-C, Lai, JH, He. A randomized controlled trial examining the effectiveness of a STOMA psychosocial intervention programme on the outcomes of colorectal patients with a stoma: study protocol. J Adv Nurs [Internet]. 2015;71(6):1310-1323. DOI: https://doi.org/10.1111/jan.12595
67. Pinto IES, Santos CSV de B, Brito MAC de, Queirós SMM. Propriedades Psicométricas do Formulário Desenvolvimento da Competência de Autocuidado da Pessoa com Ostomia de Eliminação Intestinal. Rev Enfermagem Referência [Internet]. 2016;serIV(8):75-84. DOI: https://doi.org/10.12707/RIV15044