|
Article
Gabriele Santos do Nascimento1
Vitória Ribeiro dos Santos2
Emanuella de Castro Marcolino3
Gleicy Karine Nascimento de Araújo-Monteiro4
Ana Márcia Nóbrega Dantas5
Renata Clemente dos Santos-Rodrigues6
1 ![]() https://orcid.org/0000-0002-0872-9854 UNIFACISA,
Centro Universitário, Brazil. gabriele.santos@maisunifacisa.com.br
https://orcid.org/0000-0002-0872-9854 UNIFACISA,
Centro Universitário, Brazil. gabriele.santos@maisunifacisa.com.br
2 ![]() https://orcid.org/0000-0003-3798-3453 UNIFACISA,
Centro Universitário, Brazil. vitoria.santos@maisunifacisa.com.br
https://orcid.org/0000-0003-3798-3453 UNIFACISA,
Centro Universitário, Brazil. vitoria.santos@maisunifacisa.com.br
3 ![]() https://orcid.org/0000-0002-6135-8853 UNIFACISA,
Centro Universitário, Brazil. emanuella.marcolino@maisunifacisa.com.br
https://orcid.org/0000-0002-6135-8853 UNIFACISA,
Centro Universitário, Brazil. emanuella.marcolino@maisunifacisa.com.br
4 ![]() https://orcid.org/0000-0002-4395-6518 Universidade
Federal da Paraíba, Brazil. gleicy.monteiro@maisunifacisa.com.br
https://orcid.org/0000-0002-4395-6518 Universidade
Federal da Paraíba, Brazil. gleicy.monteiro@maisunifacisa.com.br
5 ![]() https://orcid.org/0000-0001-5729-8512 Universidade
Federal da Paraíba, Brazil. amnd@academico.ufpb.br
https://orcid.org/0000-0001-5729-8512 Universidade
Federal da Paraíba, Brazil. amnd@academico.ufpb.br
6 ![]() https://orcid.org/0000-0003-2916-6832 Universidade
Federal da Paraíba, Brazil. renata.santos@maisunifacisa.com.br
https://orcid.org/0000-0003-2916-6832 Universidade
Federal da Paraíba, Brazil. renata.santos@maisunifacisa.com.br
Received: 20/05/2022
Sent to peers: 19/07/2022
Approved by peers: 01/11/2022
Accepted: 09/11/2022
Theme: Epistemology
Contribution to the subject: A conceptual analysis of phenomena found in the professional practice that contributes to advancing Nursing as a science and profession. Analyzing the concept of “Obstetric violence” assists in clarifying the phenomenon, as it treats it in detail, identifying its essential attributes, antecedents, and consequents in the Nursing context. Discussion of the theme is relevant so that Nursing professionals have subsidies to identify the cases, ensure better bonds with the patients, promote humanized, standardized, and good quality assistance, and guarantee women a dignified and safe service. In addition, it provides information and solves doubts about the theme and their rights because there is an evident need for changes in these professionals’ training and qualification in terms of the absence of procedures based on scientific evidence.
To reference this article / Para citar este artigo / Para citar este artículo: Nascimento GS, Santos VR, Marcolino EC, Araújo-Monteiro GKN, Dantas AMN, Santos-Rodrigues RC. Obstetric Violence: A Conceptual Analysis in the Nursing Context. Aquichan. 2022;22(4):e2248. DOI: https://doi.org/10.5294/aqui.2022.22.4.8
Abstract
Objective: To analyze the
concept of “Obstetric violence” in the Nursing context based on identifying its
antecedents, attributes, and consequences.
Materials and
method: It is a conceptual analysis that follows the method proposed by the Walker and
Avant model, which consists of eight stages. Six stages were used to
contemplate the study objective, namely: selection of the concept; delimitation
of the analysis objectives; identification of different uses of the concept in
the literature; determination of the essential attributes; identification of
the concept’s antecedents and consequents, and definition of the concept’s
empirical references.
Results: The sample was
comprised of 22 studies. A total of 31 antecedents were evidenced: 24
attributes for physical violence; 35 for psychological/emotional violence; 6
for institutional and sexual violence, and 5 for structural violence. Regarding
the consequences, 39 elements were found.
Conclusions: The study
contributes to Nursing science, research, and clinical practice, providing
scientific support with a deep discussion of the phenomenon and presenting the
antecedents, attributes, and consequences of obstetric violence in detail. It
enables Nursing professionals to recognize the empirical indicators of the
concept; thus, it is likely that they will have more knowledge that will lead them
to more precise Nursing care, in addition to subsidies to prevent obstetric
violence.
Keywords (Source DeCS): Nursing; concept formation; obstetric violence; violence against women; women’s health.
Resumen
Objetivo: analizar el concepto de violencia obstétrica en el marco de la
Enfermería, desde la identificación de sus antecedentes, atributos y
consecuentes.
Materiales y método: se trata de un análisis conceptual, que sigue el método planteado por
el modelo de Walker y Avant, el que consiste en ocho
etapas. Para lograr el propósito del estudio, se emplearon seis etapas:
selección del concepto; delimitación de los objetivos del análisis;
identificación de los usos del concepto en la literatura; determinación de los
atributos esenciales; identificación de los antecedentes y consecuentes del
concepto, y definición de las referencias empíricas del concepto.
Resultados: la muestra estuvo compuesta por 22 estudios. Se evidenciaron 31
antecedentes: 24 atributos para violencia física; 35, para psicológica/emocional;
6, para institucional; 6, para violencia sexual y 5, para violencia
estructural. En cuanto a los consecuentes, se encontraron 39 elementos.
Conclusiones: el estudio aporta a la ciencia de la Enfermería, la investigación y
la práctica clínica, debido a que brinda soporte científico con discusión
profunda acerca del fenómeno, además de presentar, de forma detallada, los
antecedentes, atributos y consecuentes de la violencia obstétrica. Lo anterior
posibilita al profesional de enfermería reconocer los indicadores empíricos del
concepto; así, es probable que cuente con más conocimiento que lo conduzca a
una atención en Enfermería más precisa, además de subsidios para prevenir la
violencia obstétrica.
Palabras clave (Fuente DeCS): Enfermería; formación de concepto; violencia obstétrica; violencia contra la mujer; salud de la mujer.
Resumo
Objetivo: analisar o
conceito de “violência obstétrica” no contexto da enfermagem, a partir da
identificação de seus antecedentes, atributos e consequentes.
Materiais e método: trata-se de uma análise conceitual, a qual segue o método proposto pelo
modelo de Walker e Avant, que consiste em oito etapas. Para contemplar o
objetivo do estudo, foram utilizadas seis etapas: seleção do conceito;
delimitação dos objetivos da análise; identificação dos usos do conceito na
literatura; determinação dos atributos essenciais; identificação dos
antecedentes e consequentes do conceito, e definição das referências empíricas
do conceito.
Resultados: a amostra foi composta de 22 estudos. Foram evidenciados 31
antecedentes: 24 atributos para a violência física; 35, para a
psicológica/emocional; 6, para a institucional; 6, para a violência sexual e 5,
para a violência estrutural. No tocante aos consequentes, foram encontrados 39
elementos.
Conclusões: o estudo contribui para a ciência da enfermagem, a pesquisa e a prática
clínica, uma vez que fornece suporte científico com discussão profunda do
fenômeno, apresentando, de forma detalhada, os antecedentes, atributos e
consequentes da violência obstétrica. Isso possibilita ao profissional de
enfermagem reconhecer os indicadores empíricos do conceito; assim, é provável
que ele conte com mais conhecimento que o conduza a uma assistência de
enfermagem mais precisa, além de subsídios para prevenir a violência
obstétrica.
Palavras-chave (Fonte DeCS): Enfermagem; formação de conceito; violência obstétrica; violência contra mulher; saúde da mulher.
Introduction
The obstetric violence (OV) phenomenon has several titles, such as violence during labor, cruel treatment during delivery, disrespect and abuse, institutional violence, and violence in cases of abortion and post-abortion, among others (1). The concept’s framework is not only found in the medical area but also in human rights and in other health professions. Such significant complexity generates semantic and conceptual discussions (2).
Although a complex phenomenon, it is understood OV relates to the acts of violence committed during prenatal care, at delivery, in postpartum, and during the puerperium, in which there is disrespect for women’s physical integrity and mental health, as well as loss of autonomy in terms of choices, feelings, or both (3). Since 2014, the World Health Organization (WHO) has considered OV a public health problem directly affecting women and newborns (4).
Corroborating the WHO statement, a study carried out with 409 puerperal women at a specialized comprehensive hospital in the Amhara region, northwestern Ethiopia, evidenced that three out of four (75.1%) women reported having suffered at least one type of OV during labor and delivery. The OV types were as follows: non-consensual care —260 women (63.6 %); undignified care —226 women (55.3%); physical abuse —192 women (46.9 %); non-confidential care —132 women (32.3 %); neglected care —52 women (12.7 %), and discriminated care —38 women (9.3 %) (5). It is noted that these numbers can be significantly higher due to women’s lack of understanding to identify the acts of violence, which leads to the under- reporting of cases.
The need for changes in care during pre-delivery, delivery, and birth, as well as professional training regarding the phenomenon, are essential to combat, minimize, or eradicate OV, an increasingly growing action (3).
As essential players in a woman’s prenatal, delivery, and puerperium care, nurses should guarantee comprehensive care, emotional support, commitment to health, and exchange of knowledge and experiences, in addition to having scientific knowledge focused on the needs of each pregnant woman and evidence-based practices. To promote qualified, humanized, welcoming, and systematized assistance, it is indispensable to understand the OV phenomenon (6).
Knowledge about the concept of OV needs to be expanded and improved, considering that there is no precise definition in the scientific field (7), only complementary definitions, which makes it difficult to advance the knowledge of this phenomenon and its application.
Despite the high recurrence of the phenomenon, no studies indicate its antecedents, attributes, and consequents, which hinders the professionals’ understanding, with the possibility of triggering consequences in the clinical practice (7). Thus, it becomes indispensable to clarify the concept.
That said, the study presents the following guiding question: What are the essential attributes, antecedents, and consequents to determine the concept of OV in the Nursing context? In search of answers to the question, the study aims at identifying the essential attributes, antecedents, and consequents to determine the concept of OV in the Nursing context.
Materials and Methods
This conceptual analysis followed the method proposed by the Walker and Avant model (8), which consists of eight sequential or simultaneous stages. Six stages were used in this study, as they specifically contemplated the study object, with no need to build a model case or additional cases. Each stage is described below.
· First stage: Selection of the concept — A concept that is important and useful to deepen the theoretical developments in the area of interest should be chosen.
· Second stage: Delimitation of the analysis objectives — In this stage, the researchers should define the analysis scope (8).
· Third stage: Identification of different uses of the concept in the literature — A broad literature review is done using dictionaries, thesaurus, available literature, and even friends and colleagues, identifying as many uses of the concept as possible. In this initial phase, the analysis is not restricted to a single concept aspect. There is the possibility of considering all uses of the term in question. The authors indicate that it is necessary not to limit the research merely to the medical or nursing literature, as this can influence their understanding of the true nature of the concept (8).
· Forth stage: Determination of the essential attributes — In this phase, the researchers must determine the attributes, which are words or expressions that characterize the phenomenon. In other words, they are the defining characteristics that express the phenomenon’s essence (8).
· Fifth stage: Identification of the concept’s antecedents and consequents — They are useful to further refine the attributes. The authors define ‘antecedents’ as events or incidents that must occur or be present before the occurrence of the concept and ‘consequents’ as events or incidents resulting from the occurrence of the concept. In other words, the results of the concept (8).
· Sixth stage: Definition of the concept’s empirical references — It is the final stage of concept analysis. When a concept analysis is in its concluding phase, the question is how to measure this concept or determine its existence in the real world. They are categories or classes of observable phenomena that show the occurrence of the concept using an operational definition (8).
In the first stage, the OV concept was selected considering the relevance in the professional practice and research of the authors of this study who investigate violence and vulnerability. The second stage is in line with the research objective.
The third, fourth, fifth, and sixth stages were developed simultaneously. In the third stage —Identification of the different uses of the concept in the literature, a systematic scoping literature review was carried out, as proposed by the recommendations outlined in the Joanna Briggs Institute Reviewer’s Manual (JBI [9]) and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews checklist (PRISMA-ScR [10]). The review was registered in the Open Science Framework (OSF) platform at https://osf.io/682fr/.
The research question —What are the essential attributes, antecedents, and consequents to determine the concept of OV in the Nursing context?— was determined through the PCC mnemonic, in which ‘P’ refers to participants (pregnant, parturient, and postpartum women). The first ‘C’ refers to the concept (OV, attributes, antecedents, and consequences) and the second one to the context (Nursing), following the PRISMA-ScR recommendations (10).
As for the eligibility criteria, all types of studies related to pregnant, parturient, and puerperal women addressed the theme of OV. Its attributes, antecedents, and consequents linked to the Nursing area were included. In addition, studies of any nature, available in full without a time frame and in any language, were considered, excluding duplicates indexed in more than one database.
The search followed the recommendations proposed by the JBI (9) through three stages: the first corresponds to the initial search, developed in the Theses and Dissertations Catalog of Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) and Literatura Latino-Americana e do Caribe em Ciências da Saúde (LILACS), using the following health descriptors (DeCS): gestantes (pregnant women), parto (parturition), período pós-parto (postpartum period), violência (violence), and enfermagem (nursing) with crossings using the OR and AND Boolean operators.
The second stage corresponds to the secondary search. It was conducted in the databases grouped according to the characteristics of each database, namely: LILACS (BVS), MEDLINE (PubMed), Scientific Electronic Library Online (SciELO), American Psychological Association PsycInfo and Institute of Education Sciences (ERIC), grouping the previously defined keywords. Therefore, the initial search string was as follows: (“saúde da mulher” OR parto OR “trabalho de parto” OR “parto humanizado” OR “mulheres” OR “parto obstétrico”) AND (“violência contra a mulher” OR “violência” OR “obstetrícia” OR “violações dos direitos humanos” OR “exposição à violência”) AND (“enfermagem” OR “assistência à saúde” OR “humanização da assistência” OR “enfermagem obstétrica”).
Subsequently, in the third stage, which consists of the list of references, the bibliographic references were analyzed and selected to choose the documents to be included and excluded from the study, as well as incorporating additional information.
The selection of the relevant documents was carried out by two reviewers in a paired, thorough, and independent manner. Initially, the titles and abstracts were read, excluding those papers that were incomplete or did not answer the questions established. Subsequently, the studies selected were read in full, excluding those that did not substantially portray the concept, antecedents, attributes, and consequences of OV in the Nursing context.
Any and all divergences between the reviewers were discussed to reach a consensus, considering the study eligibility criteria and methodological rigor. The selection of the corresponding words in the databases resulted in 22 final articles according to the respective crossing strategy (Figure 1).
Figure 1. Flowchart of the Summary of the Studies
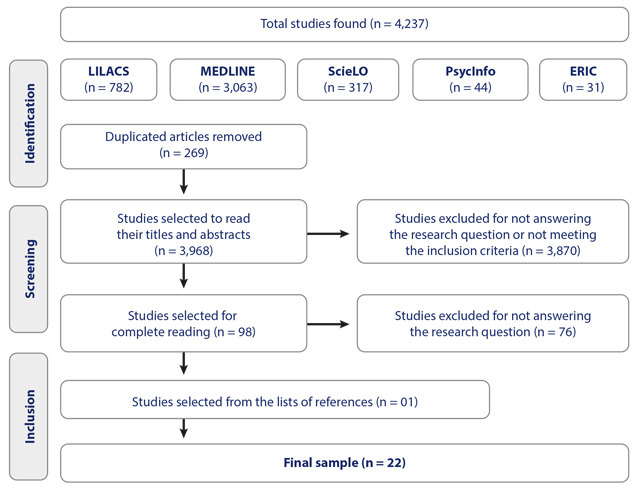
Source: Own elaboration.
After selecting the studies included to comprise the sample, the extracted data were analyzed according to the stages of determining the essential attributes, identifying the antecedents and consequents of the concept, and defining the empirical references of it.
The essential antecedents and consequents were critically analyzed and distributed according to what was addressed in the articles. The attributes were classified according to the OV typification.
Only in the last stage the OV concept was extracted from the manuscripts and transformed into a textual corpus for processing and analysis in the R Interface pour les Analyzes Multidimensionnelles de Textes et de Questionnaires (IRAMUTEQ) software. This program clearly structures the distribution of the vocabulary. By employing the similarity analysis, the results indicate the connection between the words, also distinguishing the common parts and the specificities, resulting in a maximum tree (11). Consequently, it was possible to observe the terms that operationally define the concept of OV. It is worth noting that, as it is a review, it was not necessary to submit this study to any research ethics committee.
Results
The sample comprised 22 studies from the national and international literature published in journals devoted to Nursing or other related areas between 2013 and 2021 (Table 1).
Table 1. Classification of the Articles Included in the Review
Author |
Title (in its original language) |
Year |
Type of study |
Aguiar JM, D’Oliveira AFPL, Schraiber LB (12) |
Violência institucional, autoridade médica e poder nas maternidades sob a ótica dos profissionais de saúde |
2013 |
Qualitative research |
Silva MG, Marcelino MC, Rodrigues LSP, Toro RC, Shimo AKK (13) |
Violência obstétrica na visão de enfermeiras obstetras |
2014 |
Experience report |
Souza AB, Silva LCS, Alves RN, Alarcão ACJ (14) |
Fatores associados à ocorrência de violência obstétrica institucional: uma revisão integrativa da literatura |
2016 |
Integrative literature review |
Antunes TCS(15) |
Violência obstétrica expressa no contexto das enfermeiras de uma maternidade pública do município do Rio de Janeiro |
2017 |
Descriptive, exploratory, and qualitative |
Oliveira VJ, Penna CMM(16) |
O discurso da violência obstétrica na voz das mulheres e dos profissionais de saúde |
2017 |
Interpretive, with a qualitative approach |
Zanardo GLP, Calderón M, Nadal AHR, Habigzang LF (17) |
Violência obstétrica no Brasil: uma revisão narrativa |
2017 |
Literature review |
Marrero L, Brüggemann OM (18) |
Violência institucional durante o processo parturitivo no Brasil: revisão integrativa |
2018 |
Integrative review |
Moura RCM, Pereira TF, Rebouças FJ, Costa CM, Lernades AMG, Silva LKA et al.(19) |
Cuidados de enfermagem na prevenção da violência obstétrica |
2018 |
Integrative literature review |
Perera D, Lund R, Swahnberg K, Schei B, Infanti JJ(20) |
‘When helpers hurt’: Women’s and midwives’ stories of obstetric violence in state health institutions, Colombo district, Sri Lanka |
2018 |
Field work |
Miranda FL, Velloso GS, Lima PO, Rangel SC, Almeida HF, Pinheiro MLP et al. (21) |
Violência obstétrica: percepções de enfermeiros obstétricos em uma maternidade de Minas Gerais |
2019 |
Descriptive and exploratory, with a qualitative approach |
Nascimento SL, Pires VMMM, Santos NA, Machado JC, Meira LS, Palmarella VPR (22) |
Conocimiento y vivencias de violencia obstétrica en mujeres que han vivido la experiencia del parto |
2019 |
Descriptive and of a qualitative nature |
Souza ACAT, Lucas PHCS, Lana TC, Lindner SR, Amorim T, Felisbino-Mendes MS (23) |
Obstetric violence: Integrative review |
2019 |
Integrative review |
Campos VS, Morais AC, Souza ZCSN, Araújo PO (24) |
Conventional practices of childbirth and obstetric violence under the perspective of puerperal women |
2020 |
Qualitative, descriptive, and exploratory |
Castro ATB, Rocha SP (25) |
Violência obstétrica e os cuidados de enfermagem: reflexões a partir da literatura |
2020 |
Literature review |
Menezes FR, Reis GM, Sales AAS, Jardim DMB, Lopes TC (26) |
O olhar de residentes em enfermagem obstétrica para o contexto da violência obstétrica nas instituições |
2020 |
Descriptive and exploratory, with a qualitative approach |
Mena-Tudela D, Gasch- Cervera A, Alemany-Anchel MJ, Andreu-Pejó L, Gonzálzes-Chordá VM (27) |
Design and validation of the PercOV-S Questionnaire for measuring perceived obstetric violence in nursing, midwifery and medical students |
2020 |
Instrumental design |
Pascoal KCF, Filgueiras TF, Carvalho MA, Candeia RMS, Pereira JB, Cruz RAO (28) |
Violência obstétrica na percepção de puérperas |
2020 |
Field study |
Paula E, Alves VH, Rodrigues DP, Felicio FC, Araújo RCB, Chamilco RASI et al.(29) |
Obstetric violence and the current obstetric model, in the perception of health managers |
2020 |
Descriptive and exploratory, with a qualitative approach |
Ribeiro DO, Gomes GC, Oliveira AMN, Alvarez SQ, Gonçalves BG, Acosta DF (30) |
Obstetric violence in the perception of multiparous women |
2020 |
Qualitative, of a descriptive and exploratory nature |
Silva MI, Aguiar RS (31) |
Knowledge of nurses of primary care about obstetric violence |
2020 |
Descriptive-exploratory, with a qualitative approach |
Texeira PC, Antunes LS, Duamarde LTL, Velloso V, Faria GPG, Oliveira TS(32) |
Percepção das parturientes sobre violência obstétrica: a dor que querem calar |
2020 |
Descriptive and exploratory, with a quali-quantitative approach |
Zancheta MS, Santos WS, Souza KV, Pina VR, Hwu H, Stahl H et al. (33) |
Amplifying voices on obstetric violence: Recommendations for advocacy by an obstetric nurse |
2021 |
Exploratory research |
Source: Own elaboration.
Regarding the analysis of the empirical indicators, the term ‘woman’ was identified as the most prevalent in the documents, followed by ‘autonomy,’ ‘body,’ ‘reproductive processes,’ ‘delivery,’ ‘natural process,’ ‘medicalization,’ ‘abusive,’ ‘unnecessary,’ ‘pathologization,’ ‘medication abuse,’ ‘body appropriation,’ ‘dehumanized,’ ‘postpartum,’ ‘assistance,’ ‘ability,’ ‘decision,’ ‘health professionals,’ ‘loss,’ and ‘physical integrity’ (Figure 2).

Source: IRAMUTEQ, 2021 (11).
The antecedents related to OV were organized (Table 2), representing the main risk factors that led to the occurrence of these instances. Antecedents associated with the women themselves, health professionals, institutions, and legislation were identified. The most frequent elements were ‘unfavorable financial conditions,’ ‘black-skinned women,’ and ‘lack of knowledge about the theme.’
Table 2. Concept Analysis Antecedents
Antecedents of the OV concept |
||
Elements |
Numbers of the references |
Frequency |
Unfavorable financial conditions |
10 |
|
Black-skinned women |
10 |
|
Lack of knowledge about the theme |
10 |
|
Inadequate infrastructure |
8 |
|
Lower schooling levels |
7 |
|
Unqualified professionals |
7 |
|
Naturalization and perpetuation of the practices |
6 |
|
Precariousness in terms of materials and resources |
6 |
|
Women’s lack of knowledge in relation to their sexual and reproductive rights |
5 |
|
Ethnic minorities |
5 |
|
Adolescents |
4 |
|
Work overload |
4 |
|
Non-existence of specific legislation addressing OV |
3 |
|
Lack of knowledge about own body and the delivery-physiological processes |
3 |
|
Impunity of acts |
3 |
|
Stress/Authoritarianism on the part of the professionals |
3 |
|
In abortion situation |
2 |
|
Homosexuals |
2 |
|
Inmates |
2 |
|
High number of children |
2 |
|
Immigrants |
2 |
|
Professionals’ low wages |
2 |
|
Sex workers |
(30) |
1 |
Drug users |
(30) |
1 |
Living on the street |
(30) |
1 |
Protestants |
(32) |
1 |
Single women |
(15) |
1 |
Unwanted pregnancy |
(15) |
1 |
HIV-positive women |
(15) |
1 |
Family culture |
(25) |
1 |
Women with no companion |
(30) |
1 |
Source: The authors’.
The attributes identified were organized according to the typologies (Table 3). The following terms stood out in physical violence: ‘episiotomy/episiorrhaphy,’ ‘unwarranted cesarean sections,’ ‘oxytocin use;’ in psychological/emotional violence, the most prevalent attributes highlighted were ‘humiliations’ and ‘providing false information or omitting information.’ In turn, institutional violence had the following as its main attribute: ‘not allowing the presence of a companion;’ the sexual violence typology had ‘repetitive vaginal touch examination’ as an attribute; finally, the ‘lack of human and material resources’ attribute stands out in structural violence.
Table 3. Concept Analysis Attributes
Attributes of the OV concept |
||
Physical violence |
||
Elements |
Numbers of the references |
Frequency |
Episiotomy/episiorrhaphy |
12 |
|
Unwarranted cesarean sections |
12 |
|
Oxytocin use |
9 |
|
Kristeller maneuver |
8 |
|
Lithotomy position at birth |
8 |
|
Unnecessary interventions or procedures or performed without due consent |
8 |
|
Denial of any type of pain relief |
7 |
|
Restriction to the bed |
7 |
|
Trichotomy |
7 |
|
Not using analgesics when indicated |
7 |
|
Aggressions |
6 |
|
Performance of enema |
5 |
|
Prohibition of eating or drinking |
3 |
|
Excessive medicalization |
3 |
|
Amniotomy |
3 |
|
Preventing skin-to-skin contact |
3 |
|
Trivialization of pain |
2 |
|
Use of forceps |
2 |
|
Prolonged bed rest |
2 |
|
Valsalva maneuver |
2 |
|
Causing pain |
2 |
|
Walking in the last stage of delivery |
(30) |
1 |
Not allowing immediate mother-infant contact immediately after birth |
(29) |
1 |
Invasive procedures performed on newborns that show good vitality |
(15) |
1 |
Psychological/Emotional violence |
||
Elements |
Numbers of the references |
Frequency |
Humiliations |
9 |
|
Providing false information or omitting information |
8 |
|
Threats |
7 |
|
Yelling |
6 |
|
Abandonment |
5 |
|
Disrespect |
5 |
|
Reproaches |
5 |
|
Imposition of decisions/values |
4 |
|
Rude manners |
4 |
|
Curses |
3 |
|
Disqualification of the woman’s choices |
2 |
|
Denial of care |
2 |
|
Trivialization of the woman’s suffering or needs |
2 |
|
Teasing |
2 |
|
Devaluation of women complaints |
2 |
|
Impatience |
2 |
|
Embarrassment |
(18) |
1 |
Hostile treatment |
(17) |
1 |
Irony |
(17) |
1 |
Coercion |
(17) |
1 |
Disrespect towards beliefs and cultures |
(15) |
1 |
Judgment |
(26) |
1 |
Lack of welcoming |
(29) |
1 |
Coldness |
(15) |
1 |
Harshness |
(15) |
1 |
Ironic phrases |
(26) |
1 |
Harsh speeches |
(26) |
1 |
Authoritarian behaviors |
(16) |
1 |
Derogatory words |
(16) |
1 |
Mockery |
(28) |
1 |
Moralistic speeches |
(30) |
1 |
Changes in the tone of the voice |
(23) |
1 |
Coarse treatment |
(18) |
1 |
Offenses |
(27) |
1 |
Pejorative comments |
(26) |
1 |
Institutional violence |
||
Elements |
Numbers of the references |
Frequency |
Not allowing the presence of a companion |
12 |
|
Pilgrimage in search of assistance |
3 |
|
Refusal of admission to health institutions and retention of women and their newborns in the institutions |
3 |
|
Not allowing breastfeeding |
2 |
|
Not having the opportunity to get to know the maternity ward and the professionals who will assist them |
(19) |
1 |
Difficulty accessing prenatal services or poor-quality care |
(15) |
1 |
Sexual violence |
||
Elements |
Numbers of the references |
Frequency |
Repetitive vaginal touch examination |
6 |
|
Invasion to the woman’s privacy |
4 |
|
Sexual abuse |
4 |
|
Sexual harassment |
(17) |
1 |
Unnecessary exposure of intimacy |
(30) |
1 |
Breast clinical examination without due consent and without information |
(15) |
1 |
Structural violence |
||
Elements |
Numbers of the references |
Frequency |
Lack of human and material resources |
(18) |
1 |
Inadequate infrastructure |
(18) |
1 |
Insufficient number of beds |
(18) |
1 |
Imposition of institutional routines |
(18) |
1 |
Shortage of professionals |
(12) |
1 |
Source: The authors’.
The main OV consequences found in the literature were organized (Table 4). It was observed that the interventions performed caused significant physical and psychological sequelae for women’s life and marital and maternal relationships, as well as traumas. In addition, they had consequences for the newborns, which could lead to their death. The following stand out among the consequents: ‘maternal and child morbidity and mortality,’ ‘loss of the woman’s autonomy at delivery,’ ‘emotional and psychological harms,’ and ‘physical harms.’
Table 4. Concept Analysis Consequents
Consequents of the OV concept |
||
Elements |
Numbers of the references |
Frequency |
Maternal-child morbidity and mortality |
10 |
|
Loss of the woman’s autonomy at delivery |
9 |
|
Emotional and psychological harms |
8 |
|
Physical harms |
7 |
|
Pain |
4 |
|
Repercussions for the woman’s sexual and reproductive health |
4 |
|
Negative influence on the pregnancy and delivery physiological process |
3 |
|
Third- and fourth-degree perineal laceration |
3 |
|
Infection |
3 |
|
Hemorrhage |
3 |
|
Trauma |
2 |
|
Depersonalization of the woman |
2 |
|
Urinary and fecal incontinence |
2 |
|
Fetal distress |
2 |
|
Fear |
2 |
|
Insecurity |
2 |
|
Negative effects on the mother-child bond |
2 |
|
Negative impact on women’s quality of life |
(25) |
1 |
Discrediting women and their physiological ability to give birth |
(21) |
1 |
Loss of privacy |
(16) |
1 |
Child’s developmental inability |
(28) |
1 |
Early hospitalization of women |
(32) |
1 |
It can lead to surgical delivery |
(32) |
1 |
It impairs blood flow and oxygen to the infant |
(32) |
1 |
It hinders and increases duration of labor and pain intensity during contractions |
(32) |
1 |
Low self-esteem |
(32) |
1 |
Loss of trust in the professionals |
(32) |
1 |
Tachysystole |
(24) |
1 |
Hypertonia |
(24) |
1 |
Uterine hyperstimulation, uterine rupture or both |
(24) |
1 |
Loneliness |
(18) |
1 |
Loss of the uterus |
(27) |
1 |
Stress |
(27) |
1 |
Edema |
(15) |
1 |
Episiorrhaphy endometriosis |
(15) |
1 |
It makes it difficult to initiate breastfeeding, as well as duration of exclusive breastfeeding |
(15) |
1 |
Respiratory problems for the newborn |
(15) |
1 |
Difficulty in the care targeted at the newborns and their development |
(15) |
1 |
Intensification of the difficulty to access health services |
(14) |
1 |
Source: Own elaboration.
Discussion
The expressions or terms presented using the similarity analysis evidence that the phenomenon can occur during prenatal care, delivery, the puerperium, in case of abortion, and when there are violations of the woman’s human rights and integrity, loss of autonomy and decision-making. The findings of this research point to empirical indicators that operationally define the concept of OV, which contributes to clarifying the phenomenon and providing theoretical support for nurses to timely identify the occurrence and intervene appropriately.
The category of the antecedents identifies that, for the occurrence of OV, several factors involved are related not only to the woman but to the entire pregnancy-puerperal process. The following stand out, unfavorable financial conditions, skin color, schooling level, lack of knowledge about the theme, inadequate infrastructure, precariousness in terms of materials and resources, and unqualified professionals.
Black-skinned women (12, 15, 17, 18, 20, 23, 26, 30, 32, 33) with unfavorable financial conditions (12, 15, 17, 18, 20, 23, 26, 27, 29, 30), lower schooling levels (15, 17, 20, 23, 26, 27, 32), and ethnic minorities (15, 18, 20, 27, 32) are targets more prone to violent practices, mainly routine interventions and absence of a companion. In addition, many women of low socioeconomic status with low schooling levels had limited access to prenatal consultations, which further led to disinformation about labor and delivery (34).
In a study carried out with nine low-income and black-skinned women in northeastern Brazil, physical, verbal, and institutional OV instances were reported. There were practically no reports of respect for women during delivery and minimal obstetric interventions (2).
The greater a woman’s vulnerability, the ruder and more derogatory the treatment she was offered (35). Secondly, adolescents (12, 15, 20, 30), sex workers (30), drug users (30), homeless women (30), homosexuals (15, 32), and inmates (15, 30) are more prone to negligence and omission of care (30).
A research study conducted with Chilean women evidenced that those with low schooling levels, minors, homosexuals, and indigenous reported more OV cases, mainly those treated in the public health system (36).
Lack of knowledge about the theme (15-18, 22, 25, 26, 28, 31, 32) was a significant finding of an OV antecedent. A study conducted in India with 305 women identified that 257 suffered some disrespect and abuse; of this total, 89.1% answered “no” when asked about any treatment they considered humiliating. This reveals that this type of violence is seen as something normal when knowledge is inadequate (37).
However, when understanding the act, the answers were notably different, as revealed by a survey carried out in Spain, in which 17,541 questionnaires were delivered, 38.3% realized that they had suffered OV and 44.4% perceived that they were subjected to unnecessary or painful procedures, of which 83.4% were not asked for their due informed consent (7).
Naturalization and perpetuation of the practices (12, 15, 17, 24-26), an OV antecedent, such as pain related to delivery (38), is also associated with a lack of knowledge on the topic. It is believed that delivery is a painful process, naturalizing the unfavorable situations experienced by the women and not recognizing some procedures as violence but common and routine situations (39).
Knowledge about the body and the physiology of delivery favors the reduction of vulnerability, the fight against OV and women’s empowerment, ensuring their rights and autonomy and counteracting abusive actions performed by professionals.
The following stand out among the antecedents related to health professionals and institutions: unqualified professionals (14, 15, 21, 22, 26, 27, 29), work overload (14, 20, 23, 26), the professionals’ low wages (14, 16), stress/authoritarianism on the part of the professionals (15, 23, 30), inadequate infrastructure (13-16, 20, 21, 23, 26), precariousness in terms of materials and resources (12, 14, 15, 23, 26, 33) and impunity of acts (12, 16, 21). Due to a lack of training and adequate working conditions —especially associated with insufficient materials and resources, obstetric care quality becomes increasingly dehumanized, causing emotional stress and overload in professionals (40).
The professionals’ inability to offer qualified assistance, which allows for predicting violence and intervening, reflects a society that has always naturalized violent behaviors and procedures as non-violent. In addition, the professional-user hierarchy, with unilateral authority, tends to lead professionals to verbalize and perform violent techniques or both without noticing that they are, in fact, violent (41). Therefore, it is fundamental that professionals know the OV antecedents, attributes, and consequents to provide good quality care throughout the pregnancy-puerperal process.
The attributes, which are essential characteristics of the phenomenon, were grouped according to the type of violence into physical, psychological or emotional, institutional, sexual, and structural, which allowed for a better understanding of OV.
Among the attributes included in the category of physical OV, interventions and procedures that are unnecessary or performed without due consent (14, 15, 17, 21, 27, 28, 30, 33) stand out, as well as oxytocin use (13, 15, 18, 22-26, 32), episiotomy and episiorrhaphy (13, 14, 17, 18, 20, 22-26, 28, 32), Kristeller maneuver (15, 18, 22, 23, 25-27, 32), constant use of forceps (25, 32), denial of any type of pain relief (14, 17, 18, 25, 29, 30, 32) whether by means of non-pharmacological methods or not, restriction to the bed (18, 23, 24-26, 29, 30), prohibition of eating or drinking (23, 25, 32), enema (15, 17, 22, 25, 28), trichotomy (17, 22, 23, 25, 26, 30, 32), which includes unnecessary removal of pubic hair, and mandatory lithotomy position at birth (17, 18, 23-25, 28, 29, 32), which causes increased pain and slows down the delivery process.
These attributes are mentioned in several interviews with women in maternity hospitals in the Czech Republic (42). In another research study carried out in a hospital in Azuay, Ecuador, the women also reported these attributes they characterized as types of physical violence (43). These studies corroborate the results found in the current one, validating the essence of the phenomenon.
Some women point out another perception about the Kristeller maneuver and oxytocin administration. In a research study carried out with 57 puerperal women in the central area of the Huasteca region of San Luis Potosí, Mexico, it was reported that these procedures are an act of gratitude towards the mothers at delivery, as they help the infant to descend more quickly and minimize moments of prolonged suffering (44).
However, when episiotomy and episiorrhaphy were mentioned (44), the women’s reports of actually feeling OV were unanimous, mainly in cases where they were not informed. This agreement is observed in several pieces of scientific evidence (16, 43, 44).
Despite the efforts to seek humanization in obstetric care, the following is clearly noticeable: predominance of interventional procedures such as excessive medicalization (14, 17, 21), trivialization of the pain felt by the women (20, 30), not using analgesics when indicated (12, 15, 16, 21, 27, 31, 33), forcing parturient women to walk in the last stage of delivery (30) without their consent, prolonged bed rest (22, 32), aggressiveness (12, 14, 15, 18, 24, 27), and performing an amniotomy (23, 24, 32) and the Valsalva maneuver (23, 24), which refers to encouraging voluntary push, with unequal power relations between professionals and women prevailing (16).
Physical violence is more prevalent because it is more easily identifiable among women, as shown by a research study carried out at a public hospital in North Shewa, Amhara, Ethiopia. It was pointed out that 100% (435) of the women identified some of these attributes that characterize OV related to physical characteristics (45).
The following attributes stand out in the psychological OV category: humiliation (14, 17, 18, 23, 25, 27, 28, 31, 32), teasing (15, 17), providing false information or omitting information (15, 18, 19, 23, 24, 29, 30, 32), yelling (14, 16, 18, 25, 31, 32), threats (16, 18, 25, 28, 30-32), disqualification of women’s decisions (18, 30), denial of care (18, 26), abandonment (18, 20, 24, 26, 32), embarrassment (18), imposition of decisions/values (15, 18, 19, 26), trivialization of women’s suffering or needs (18, 20), reproaches (14, 16, 18, 31, 32), ironic phrases (17), and coldness (15).
The harms caused by psychological OV go beyond the physical aspect, leaving emotional and psychological scars for a long time, undermining the emotional realm and bringing about consequences that negatively interfere with the puerperal period, a delicate moment for puerperal women (46). It should be noted that these problems can lead to postpartum depression (47).
In an analysis of the notifications of pregnant women in Brazil between 2011 and 2018, with 2,033,026 cases, the type of violence with the highest incidence was physical (61.9 %), followed by psychological (31.2 %) and lastly, sexual (27 % (48)).
The incidence of reports that mention the essential characteristics of the phenomenon, that is, the attributes, is considerably high. A multicenter survey carried out in the United States with 2,138 women indicates that one out of six (17.3 %) mentions some type of abuse, such as yelling, disrespect, unknown or erroneous information, denial of care, embarrassment, and loss of decision-making autonomy. It is believed that more women have suffered psychological violence, although they could not identify it (49).
From the institutional category perspective, the attribute with the highest incidence was not allowing the presence of a companion (12, 14, 15, 17, 23-26, 28, 29, 32, 33). Brazilian women are supported by the Companion Law (Law 11,108) of April 7th, 2005, which allows for the presence of a companion during delivery, childbirth, and the immediate postpartum period, either in private or public health services (50).
Although supported by law, qualitative studies (51, 52) still notice reports of Brazilian women who claimed they were not allowed to have a companion and accepted so due to lack of information, even with distress.
In the sexual OV category, the most characteristic attributes were a repetitive vaginal touch (15, 18, 22, 25, 28, 32), invasion of privacy (17, 26, 27, 33), sexual abuse (17, 30-32), and unnecessary exposure of intimacy (30).
Repeatedly touching the vagina can cause harm, such as inciting premature birth and infection in the infant (53) and inducing pain and discomfort. In a study, Mexican women mentioned that they feel unnecessarily invaded in their privacy and exposed, with several touches practically at the same time, reporting that there seems to be no communication between the health professionals (44).
A shocking report in a research study conducted in northern Brazil reveals that the health professional performed the vaginal touch examination and asked all the students present to repeat the procedure, causing discomfort, invasion of privacy and exposure of the woman’s intimacy (53). This scenario proves to be totally inhuman to the woman.
That is a reality not only in Brazil but also in other countries, such as Iran, where the prevalence of sexual OV stands out in relation to the other types. This assertion is indicated in a study conducted with 725 women, in which 14.8% suffered sexual violence, 9.9% were victims of psychological violence, and 6.5% of physical violence. Domestic sexual abuse was also very evident (48).
Finally, the structural OV attributes refer to precarious assistance or omission to the detriment of the infrastructure (18), lack of human and material resources (18), lack of beds (18), imposition of institutional routines (18) and shortage of professionals (12). This is more likely to occur in public institutions before the woman’s hospitalization, affecting both her and the professionals, which entails overload and undignified working conditions (18).
These attributes are proven through diverse evidence in practice. During data collection, nurse-researchers noticed a deficit in terms of equipment and a lack of necessary maintenance, especially in the public sector, in addition to communication difficulties between professionals and the absence of adequate signs in the environment (14).
In the category of the OV phenomenon consequents, resulting events or incidents were detected, such as loss of women’s autonomy, emotional and psychological harms, and maternal and child morbidity and mortality.
When a woman loses her autonomy during delivery (15-17, 23-26, 29, 32), her primary role is obliterated, in addition to her decision-making power. For this gap, it is recommended that women look for a support network during prenatal care to acquire knowledge (54).
The formation of groups of pregnant women in southern Brazil showed that those who regularly participated in the meetings were able to enjoy significant autonomy and were willing to argue and impose their wishes, showing greater awareness of the delivery moment (55).
Other terms presented as OV consequents were emotional and psychological harms (12, 14, 22, 25-28, 32), fear (15, 18), insecurity (15, 18) and loneliness (18).
These terms corroborate a research study conducted in northeastern Brazil, in which the puerperal women mentioned having suffered emotional and psychological consequences, resulting in frustration, anger, anguish, and impotence. In the interviews, it is possible to see hints of postpartum depression and trauma after the episiotomy procedure. Consequently, the same women reported that these problems affected their sex lives (52).
In the findings of the current study, episiotomy, an OV attribute, refers to the following consequences: third- and fourth-degree perineal laceration (14, 15, 22), infection (14, 15, 22), intense bleeding (14, 15, 22), urinary and fecal incontinence (14, 22), edema (15), and episiorrhaphy endometriosis (15). Although uncommon, episiorrhaphy endometriosis is more prevalent in women who have undergone at least one episiotomy and in cases of vaginal deliveries with curettage to avoid hemorrhages and uterine subinvolution (56).
Procedures considered routine and standardized in health services, without indication, can cause or intensify pain (15, 26, 27, 32), physical harm (12, 14, 26-28, 30, 32), and unnecessary suffering. In view of this, the importance of dialogue between professionals, especially nurses, and pregnant women is emphasized, in addition to providing fundamental information about the pregnancy-puerperal process and encouraging self-knowledge about their bodies, role, and decision-making power (57).
An important OV consequence is maternal and child morbidity and mortality (13-17, 19, 25, 26, 28, 30) during labor and the puerperium, mainly due to cesarean sections without indication, which intensifies the likelihood of respiratory problems for the newborn (15) and triples the mother’s mortality risk, in addition to the possibility of also causing loss of the uterus (27).
OV can lead to maternal morbidity and mortality due to several factors, such as adverse events related to aggressive management of vaginal and cesarean deliveries, neglect to perceive the suffering experienced by the woman, hostility, negligence, and delay in assisting women who are having an abortion —spontaneous or desired— and not allowing the presence of a companion (51).
Finally, it is crucial that nurses are aware of the OV phenomenon and duly trained and able to identify it and intervene in a timely manner, offering humanized, comprehensive, empathetic, and qualified assistance.
It is believed that this concept analysis contributes to Nursing science, research, and clinical practice, considering that it provides scientific support with a deep discussion of the phenomenon, presenting the OV antecedents, attributes, and consequents in detail. This enables nurses to recognize the empirical indicators of the concept; thus, it is likely that they will have a greater knowledge that will lead them to more precise Nursing care in the clinical practice.
As a limitation, we cite non-elaboration of the model case and additional cases; however, there was an in-depth analysis of empirical bases and compliance with methodological rigor.
Conclusions
In this research, it was possible to analyze the OV concept, identifying 76 related attributes, 31 antecedents, and 39 consequents. The study made it possible to contribute greater clarity to the phenomenon, offering theoretical and scientific support for nurses to identify OV cases and contributing to the evolution of Nursing epistemology.
The multidimensionality of the topic studied was comprehensively observed, as it presents several typifications, each with their respective essential characteristics, in addition to their multiple antecedents and consequents in the scenario of OV during the pregnancy-puerperal period.
Conflict of interest: None declared.
Funding: There were no funding sources.
References
1 Mena- Tudela D, Cervera-Gasch A, Andreu-Pejó L, Alemany-Anchel MJ, Valero-Chillerón MJ, Peris-Ferrando E et al. Perception of obstetric violence in a sample of Spanish health sciences students: A cross-sectional study. Nurse Educ Today. 2022;110:105266. DOI: https://doi.org/10.1016/j.nedt.2022.105266
2. Lima KD, Pimentel C, Lyra TM. Disparidades raciais: uma análise da violência obstétrica em mulheres negras. Ciênc Saúd Coletiva. 2021;26(3):4909-18. DOI: https://doi.org/10.1590/1413-812320212611.3.24242019
3. Martín-Badia J, Obregón-Gutiérrez N, Goberna-Tricas J. Obstetric violence as an infringement on basic bioethical principles. Reflections inspired by focus groups with midwives. Int J Environ Res Public Health. 2021;18(23):12553. DOI: https://doi.org/10.3390/ijerph182312553
4. Organização Mundial da Saúde. Prevenção e eliminação de abusos, desrespeito e maus-tratos durante o parto em instituições de saúde. Genebra: Departamento de Saúde Reprodutiva e Pesquisa/OMS; 2014. Disponível em: https://apps.who.int/iris/bitstream/handle/10665/134588/WHO_RHR_14.23_por.pdf?sequence=3
5. Mihret MS. Obstetric violence and its associated factors among postnatal women in a Specialized Comprehensive Hospital, Amhara Region, Northwest Ethiopia. BMC Res Notes. 2019;12(1):600. DOI: https://doi.org/10.1186/s13104-019-4614-4
6. Alexandría ST, Oliveira MSS, Alves SM, Bessa MMM, Albuquerque GA, Santana MDR. La violencia obstétrica bajo la perspectiva de los profesionales de enfermería involucrados en la asistencia al parto. Cultura de los Cuidados (edición digital). 2019;23(53). DOI: https://doi.org/10.14198/cuid.2019.53.12
7. Mena-Tudela D, Iglesias-Casás S, González-Chordá VM, Cervera-Gasch Á, Andreu-Pejó L, Valero-Chilleron MJ. Obstetric violence in Spain (Part I): Women’s perception and interterritorial differences. Int J Environ Res Public Health. 2020;17(21):7726. DOI: https://doi.org/10.3390/ijerph17217726
8. Walker LO, Avant KC. Strategies for theory construction in nursing. 6ª edição. Pearson; 2019.
9. Aromataris E, Munn Z. JBI manual for evidence synthesis [Internet]. JBI; 2020. DOI: https://doi.org/10.46658/JBIMES-20-01
10. Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169(7):467-73. DOI: https://doi.org/10.7326/M18-0850
11. Ratinaud, P. IRAMUTEQ: Interface de R pour les analyses multidimensionnelles de textes et de questionnaires [software]. 2009. Disponível em: http://www.iramuteq.org/
12. Aguiar JM, D’Oliveira AFPL, Schraiber LB. Violência institucional, autoridade médica e poder nas maternidades sob a ótica dos profissionais de saúde. Cad Saúde Pública [Internet]. 2013;29(11):2287-96. DOI: https://doi.org/10.1590/0102-311x00074912
13. Silva MG, Marcelino MC, Rodrigues LSP, Toro RC, Shimo AKK. Obstetric violence according to obstetric nurses. Rev Rene [Internet]. 2014;15(4):720-8. DOI: https://doi.org/10.15253/2175-6783.2014000400020
14. Souza AB, Silva LC, Alves RN, Alarcão ACJ. Fatores associados à ocorrência de violência obstétrica institucional: uma revisão integrativa da literatura. Rev ciênc méd [Internet]. 2016; 25(3):115-28. DOI: https://doi.org/10.24220/2318-0897v25n3a3641
15. Antunes TCS. A violência obstétrica expressa no contexto das enfermeiras de uma maternidade pública do município do Rio de Janeiro [dissertação]. Rio de Janeiro: Faculdade de Enfermagem, Universidade do estado do Rio de Janeiro; 2017. Disponível em: https://www.bdtd.uerj.br:8443/handle/1/11431#preview-link0
16. Oliveira VJ, Penna CMM. Discussing obstetric violence through the voices of women and health professionals. Texto & Contexto Enfermagem. 2017;26(2):e06500015. DOI: https://doi.org/10.1590/0104-07072017006500015
17. Zanardo GLP, Uribe MC, Nadal AHR, Habigzang LF. Violência obstétrica no Brasil: uma revisão narrativa. Psicol & Soc. 2017;29:e155043. DOI: https://doi.org/10.1590/1807-0310/2017v29155043
18. Marrero L, Brüggemann OM. Institutional violence during the parturition process in Brazil: Integrative review. Rev Bras Enferm. 2018;71(3):1152-61. DOI: https://doi.org/10.1590/0034-7167-2017-0238
19. Moura RCM, Pereira TF, Rebouças FJ, Costa CM, Lernades AMG, Silva LKA et al. Cuidados de enfermagem na prevenção da violência obstétrica. Enferm Foco. 2018;9(4):60-5. DOI: https://doi.org/10.21675/2357-707X.2018.v9.n4.1333
20. Perera D, Lund R, Swahnberg K, Schei B, Infanti JJ. ‘When helpers hurt’: Women’s and midwives’ stories of obstetric violence in state health institutions, Colombo district, Sri Lanka. BMC Pregnancy Childbirth. 2018;18(1):1-12. DOI: https://doi.org/10.1186/s12884-018-1869-z
21. Miranda FL, Velloso GS, Lima PO, Rangel SC, Almeida HF, Pinheiro MLP et al. Violência obstétrica: percepções de enfermeiros obstétricos em uma maternidade de Minas Gerais. HU Rev [Internet]. 2019;45(4):415-20. DOI: https://doi.org/10.34019/1982-8047.2019.v45.27818
22. Nascimento SL, Pires VMMM, Santos NA, Machado JC, Meira LS, Palmarella VPR. Conocimiento y vivencias de violencia obstétrica en mujeres que han vivido la experiencia del parto. Enfermería Actual de Costa Rica. 2019;37:66-79. Disponible en: https://www.scielo.sa.cr/scielo.php?pid=S1409-45682019000200066&script=sci_abstract&tlng=es
23. Souza ACAT, Lucas PHCS, Lana TC, Lindner SR, Amorim T, Felisbino-Mendes MS. Violência obstétrica: uma revisão integrativa. Rev. enferm. UERJ. 2019;27:e45746. DOI: https://doi.org/10.12957/reuerj.2019.45746
24. Campos VS, Morais AC, Souza ZCSN, Araújo PO. Práticas convencionais do parto e violência obstétrica sob a perspectiva de puérperas. Rev Baiana Enferm. 2020; 34:e35453. Disponível em: http://www.revenf.bvs.br/scielo.php?script=sci_arttext&pid=S2178-86502020000100323
25. Castro ATB, Rocha SP. Violência obstétrica e os cuidados de enfermagem: reflexões a partir da literatura. Enferm Foco 2020;11(1):176-81. DOI: https://doi.org/10.21675/2357-707X.2020.v11.n1.2798
26. Menezes FR, Reis GM, Sales AAS, Jardim DMB, Lopes TC. O olhar de residentes em enfermagem obstétrica para o contexto da violência obstétrica nas instituições. Interface - Comunicação, Saúde, Educação. 2020;24:e180664. DOI: https://doi.org/10.1590/interface.180664
27. Mena-Tudela D, Gasch- Cervera A, Alemany-Anchel MJ, Andreu-Pejó L, Gonzálzes-Chordá VM. Design and validation of the PercOV-S questionnaire for measuring perceived obstetric violence in nursing, midwifery and medical students. Int J Environ Res Public Health. 2020;17 (21):8022. DOI: https://doi.org/10.3390/ijerph17218022
28. Pascoal KCF, Carvalho MA, Candeia RMS, Pereira JB, Cruz RAO, Filgueiras TF. Violência obstétrica na percepção de puérperas. Rev Nursing. 2020;23(265):4221-32. DOI: https://doi.org/10.36489/nursing.2020v23i265p4221-4232
29. Paula E, Alves VH, Rodrigues DP, Felicio FC, Araújo RCB, Chamilco RASI et al. Obstetric violence and the current obstetric model, in the perception of health managers. Texto & Contexto - Enferm. 2020;29:e20190248. DOI: https://doi.org/10.1590/1980-265x-tce-2019-0248
30. Ribeiro DO, Gomes GC, Oliveira AMN, Alvarez SQ, Gonçalves BG, Acosta DF. Obstetric violence in the perception of multiparous women. Rev Gaúcha Enferm. 2020;41:e20190419. DOI: https://doi.org/10.1590/1983-1447.2020.20190419
31. Silva MI, Aguiar RS. Conhecimento de enfermeiros da atenção primária acerca da violência obstétrica. Rev Nursing. 2020;23(271):5013-24. DOI: https://doi.org/10.36489/nursing.2020v23i271p5013-5024
32. Texeira PC, Antunes LS, Duamarde LTL, Velloso V, Faria GPG, Oliveira TS. Percepção das parturientes sobre violência obstétrica: a dor que querem calar. Rev Nursing. 2020;23(261):3607-15. DOI: https://doi.org/10.36489/nursing.2020v23i261p3607-3615
33. Zancheta MS, Santos WS, Souza KV, Pina VR, Hwu H, Stahl H et al. Ampliando vozes sobre violência obstétrica: recomendações de advocacy para enfermero obstetra. Esc Anna Nery Rev Enferm. 2021;25(5):e20200449. DOI: https://doi.org/10.1590/2177-9465-ean-2020-0449
34. Davis DA. Obstetric racism: The racial politics of pregnancy, labor, and birthing. Med Anthropol. 2019;38(7):560-73. DOI: https://doi.org/10.1080/01459740.2018.1549389
35. Wado YD, Mutua MK, Mohiddin A, Ijadunola MY, Faye C, Coll CVN, et al. Intimate partner violence against adolescents and young women in sub-Saharan Africa: Who is most vulnerable? Reproductive Health [Internet]. 2021;18(1):1-13. DOI: https://doi.org/10.1186/s12978-021-01077-z
36. Castro MC, Rates SS. Violencia obstétrica en Chile: percepción de las mujeres y diferencias entre centros de salud. Rev Panam Salud Publica. 2022;46:e24. DOI: https://doi.org/10.26633/RPSP.2022.24
37. Nawab T, Erum U, Amir A, Khalique N, Ansari MA, Chauhan A. Disrespect and abuse during facility-based childbirth and its sociodemographic determinants: A barrier to healthcare utilization in rural population. J Family Med Prim Care. 2019;8(1):239-45. DOI: https://doi.org/10.4103/jfmpc.jfmpc_247_18
38. Ayala PM. Violencia obstétrica: reproduciendo el dolor. Via Inveniendi Et Iudicandi. 2021;16(2): 1-29. DOI: https://doi.org/10.15332/19090528.6783
39. Leite TH, Marques ES, Esteves-Pereira AP, Nucci MF, Portella Y, Leal MC. Desrespeitos e abusos, maus tratos e violência obstétrica: um desafio para a epidemiologia e a saúde pública no Brasil. Ciênc Saúd Coletiva. 2022;27(2):483-91. DOI: https://doi.org/10.1590/1413-81232022272.38592020
40. Shrivastava S, Sivakami M. Evidence of ‘obstetric violence’ in India: An integrative review. Biosoc Sci. 2020;52(4):610-28. DOI: https://doi.org/10.1017/S0021932019000695
41. Mir JR, Gandolfi AM. La violencia obstétrica: una práctica invisibilizada en la atención médica en España. Gaceta Sanitaria. 2021;35(3):211-2. DOI: https://doi.org/10.1016/j.gaceta.2020.06.019
42. Begley C, Sedlicka N, Daly D. Respectful and disrespectful care in the Czech Republic: An online survey. Reprod Health. 2018;15(1):198. DOI: https://doi.org/10.1186/s12978-018-0648-7
43. Palacios DCV, Cárdenas TXC, Peñaranda DAL, Torres ZKS, Johanna PÁN. Obstetric violence by health personnel from the perspective of women who attend a hospital in Azuay, Ecuador. Investigación Clínica. 2020;61:140-51. Available at: https://www.scopus.com/record/display.uri?eid=2-s2.0-85101278826&origin=inward&txGid=37d23473de8a526d5bfe5d883f86ab95
44. Flores YYR, Ledezma AGM, Ibarra LEH, Acevedo CEG. Construcción social de la violencia obstétrica en mujeres Tének y Náhuatl de México. Rev da Escola Enfermagem USP. 2019;53:e03464. DOI: https://doi.org/10.1590/s1980-220x2018028603464
45. Adinew YM, Hall H, Marshall A, Kelly J. Disrespect and abuse during facility-based childbirth in central Ethiopia. Global health action. 2021;14(1):1923327. DOI: https://doi.org/10.1080/16549716.2021.1923327
46. Scandurra C, Zapparella R, Policastro M, Continisio GI, Ammendola A, Bochicchio V et al. Obstetric violence in a group of Italian women: Socio-demographic predictors and effects on mental health. Cult Health Sex. 2021 31:1-15. DOI: https://doi.org/10.1080/13691058.2021.1970812
47. Chisholm CA, Bullock L, Ferguson JEJ. Intimate partner violence and pregnancy: Epidemiology and impact. Am J Obstet Gynecol. 2017;217(2):141-4. DOI: https://doi.org/10.1016/j.ajog.2017.05.042
48. Colonese CF, Pinto LW. Analysis of reports of violence against pregnant women in Brazil in the period from 2011 to 2018. Texto & Contexto Enferm. 2022;31:e20210180. DOI: https://doi.org/10.1590/1980-265x-tce-2021-0180
49. Vedam S, Stoll K, Taiwo TK, Rubashkin N, Cheyney M, Strauss N et al. The Giving Voice to Mothers study: Inequity and mistreatment during pregnancy and childbirth in the United States. Reprod Health. 2019;16(1):1-18. DOI: https://doi.org/10.1186/s12978-019-0729-2
50. Brasil. Lei nº 11.108 de 7 de abril de 2005. Altera a Lei 8.080, de 19 de setembro de 1990, para garantir às parturientes o direito à presença de acompanhante durante o trabalho de parto, parto e pós-parto imediato, no âmbito do Sistema Único de Saúde — SUS. Diário Oficial da União [Internet]. Brasília (DF); 8 abril 2005. Disponível em: https://presrepublica.jusbrasil.com.br/legislacao/96776/lei-11108-05
51. Diniz SG, Salgado HO, Andrezzo HFA, Carvalho PGC, Carvalho PCA, Aguiar CA et al. Abuse and disrespect in childbirth care as a public health issue in Brazil: Origins, definitions, impacts on maternal health, and proposals for its prevention. Rev Bras Crescimento Desenvolv Hum Development. 2015;25(3):377-82. DOI: https://doi.org/10.7322/jhgd.106080
52. Rocha MJ, Grisi EP. Violência obstétrica e suas influências na vida de mulheres que vivenciaram essa realidade. Revista de psicologia [Internet]. 2017;11(38):623-35. DOI:
53. Goes CS, Almeida JS, Silva PA, Lopes GS, Rodrigues MEA, Santos AM. Perceptions of postpartum women about obstetric violence in a maternity hospital in Manaus. Res Soc Dev. 2021;10(15):e381101522670. DOI: https://doi.org/10.33448/rsd-v10i15.22670
54. Jamieson B. Exposure to interpersonal violence during pregnancy and its association with women’s prenatal care utilization: A meta-analytic review. Trauma Violence Abuse. 2020;21(5):904-21. DOI: https://doi.org/10.1177/1524838018806511
55. Gashaw BT, Magnus JH, Schei B. Intimate partner violence and late entry into antenatal care in Ethiopia. Women Birth. 2019;32(6):e530-7. DOI: https://doi.org/10.1016/j.wombi.2018.12.008
56. Valencia MH, Zárate A, Quijano TH, Oca MELM, Godínez GE. Endometriosis in delayed scarring of postpartum eutocic episiorrhaphy. Integral aspects and a case report. Rev Med Inst Mex Seguro Soc. 2005;43(3):237-42. Available at: https://pubmed.ncbi.nlm.nih.gov/16138458/
57. Shimoda K, Leshabari S, Horiuchi, S. Self-reported disrespect and abuse by nurses and midwives during childbirth in Tanzania: A cross-sectional study. BMC Pregnancy Childbirth. 2020;20(1):584. DOI: https://doi.org/10.1186/s12884-020-03256-5