Introduction
Newborns who have complications related to prematurity, such as cerebral palsy, hemorrhages,
and infections, which need prolonged periods of hospitalization, are at greater risk
of death and developing special health needs 1,2. Newborns weighing less than 1,000 grams, gestational age less than 28 weeks and
Apgar score at birth below seven are recognized as factors that can potentiate complications
and special health needs in the long term 2. Children with Special Health Needs (CSHN) are those who are at high risk of evolving
with chronic, physical, developmental, behavioral, or emotional conditions and require
additional health services to those offered to children of the same age 3.
The costs generated by a baby who requires hospitalization are not only financial,
but they also involve psychological costs for the child and the families involved,
as there can be harmful effects on cognitive and emotional development throughout
their life because they need specialized care and/or supplies 4,5. This situation demands changes in the role of parents and influences the ability
for healthy parenting.
In the presence of premature newborns with special health needs, at birth or during
hospitalization, there is an urgency in the recognition of demands from families and
health professionals to guarantee qualified monitoring of their development 6,7. Thus, it is essential that mothers recognize these health needs, as they are the
ones who can provide positive experiences and stimuli most of the time to strengthen
the baby's development in the home environment with the family, with the help of a
trained professional network 8,9. The present study formulated the research questions: Do premature newborns have
the potential to develop special health needs? and, are these potentialities perceived
from maternal concerns?
Furthermore, by recognizing the relevance and the primordiality of comprehensive care
for children prematurely born, the choice for the triangulation of methods in this
study is justified by the complex nature of the phenomenon of special health needs,
understanding that they can be of clinical origin and suffer interference from intervening
elements of different natures.
To answer the research questions, this study aimed to identify premature newborns
with potential risk factors to develop special health needs and describe the maternal
recognition of these factors.
Methods
This study used a triangulation of methods articulating the approaches in a complementary
way; it valued the qualitative and the quantitative, understood as an indicator and
a part of the deepening of the phenomena 10. The study was conducted in Foz do Iguaçu-PR, Southern Brazil, a city on the triple
border (Brazil-Paraguay-Argentina), from July 2017 to May 2018. The population for
the study was composed of all children born with a gestational age of less than 37
weeks and hospitalized in the Neonatal Intensive Care Unit (NICU), regardless of the
mother's place of origin. Premature children who remained hospitalized at a later
date than that of the data collection were excluded. The final sample was composed
of 951 premature babies.
Participants were living in the city of Foz do Iguaçu, Paraná State (PR), Brazil,
over 18 years old, and were independently selected, for convenience, from the quantitative
sample in the period from July to October 2017. Mothers with a diagnosis of mental
health problems registered in medical records and those where there was an inability
to perform home visits (no location of the address and / or absence of the mother
at the address) after three attempts were excluded. The invitation to participants
ended when the data collected began to respond to the objectives of this study. In-depth
interviews were conducted with 18 mothers of 20 children (two are twins), who were
born premature and remained hospitalized in the NICU.
Data collection occurred concurrently and throughout the analysis. The results of
the quantitative study were incorporated, supporting the analysis of the database
in the qualitative stage. Potential factors for the development of special health
needs among preterm infants discharged from the NICU were assumed as a guiding structure
and a theory was implicit.
In the quantitative approach, a cross-sectional study was conducted, with retrospective
data collection, which analyzed all the medical records of hospitalizations of premature
newborns in the period from 2013 to 2017. The search for the data took place in the
archives sector of a hospital that is a reference for high-risk pregnancy and neonatology.
The data collection instrument consisted of a structured script, organized by the
researchers, who have experience in neonatology studies, which was built based on
previous research results 3,11,12, so, it wasn't a validated instrument. The variables were categorized into birth
weight (≤ 1,000g, 1,001-1,500g, 1,501-2,499g, 1,500-3,999g, ≥ 4,000g); gestational
age (<28, 28-31, 32-33, 34-36 weeks); Apgar score in the 1st and 5th minute (<7, ≥
7); complications with the newborn (yes or no); number of days of Mechanical Ventilation
(MV) and hospitalization (<7, 7 days or more).
The qualitative approach was built based on philosophical hermeneutics, a framework
that is comprehensive and interpretive of the content permeating human experience,
rooted in processes and acts mediated by dialogue 13. This qualitative stage was organized into four meetings. At the first meeting at
the hospital, mothers were approached when they arrived to visit and/or breastfeed
their children, who were already in the NICU.
At the time of data collection, the visitation policy remained in the institution.
This initial approach took place in the waiting/breastfeeding room, where the mothers
were invited to participate and, after their consent, the signature of the Free and
Informed Consent Form (ICF) was collected. This moment was important for the interaction
between participant-researcher, and for the application of the "CSHN Screening" script
3 -also used in other research meetings, which sought to describe the maternal recognition
of the need for medication, the use of services and the functional limitations of
the premature child.
The second meeting took place through a Home Visit (HV), held 15 days after the baby
was discharged from the hospital, with an interview directed by the guiding question:
"Tell me about the daily care of your child?". The interviews, carried out by a nurse
with professional experience in neonatology, took place at the participant's own home
at a time chosen by them, having an average duration of 40 minutes, recorded on audio,
and transcribed in full, with feedback to the participants for validation of the transcription
of the interviews.
For the third and fourth meetings, two contacts were made by telephone or by text
message (30 days after the HV and when the child reached six months of age). In these
contacts, we sought to identify the special health needs presented by the child at
home and to verify possible changes in the child's development and behavior. To assess
the changes (after six months of the child's birth), questions were organized for
the telephone interview adapted from two instruments, the Survey of Well-being of
Young Children (SWYC), and the Baby Pediatric Symptom Checklist (BPSC) 14, instruments have been validated in Brazil. The SWYC has the purpose of screening
behavioral and developmental disorders in children, according to each age group, as
observed by the mothers. This checklist considers the options: Does not do, does a
little or does a lot, and for each answer points are assigned between zero, one and
two, respectively, adding them up at the end. The instrument assigns values to the
scores, indicating whether the child is at risk or not. At the assessment at six months
of age, the SWYC considers that a value greater than 11 indicates the child is not
at risk, but if it is equal to or below 11 the child needs additional assessment 14.
The BPSC seeks to perform a screening that identifies behavioral symptoms, divided
into three subscales (four items each), with scores between zero and two, in the same
proportion: Does not do, does a little, or does a lot. The total score of one of the
three sub-scales greater than or equal to three suggests risk 14. These screening instruments allow us only to identify whether the child presents
risks or not that may compromise the child's development and behavior. However, these
are not definers of diagnostics, and the participants were instructed to seek health
services for evaluation.
A descriptive statistical analysis of the data was done, using the Chi-square test;
the p-value considered statistically significant was <0.05. Data analysis was performed
using the SPSS 23.0 program. The variables length of hospitalization, gestational
age, birth weight, Apgar score at 1st and 5th minute and complications were evaluated
using the Pearson Correlation.
The analysis of the interviews was undertaken through the interpretation of meanings,
which describe and contextualize information based on interviews, culminating in themes
that portray significant parts of the data set. In this way, repeated readings of
the material were performed, with a view of the whole context and its particularities,
seeking to understand the meanings and reinterpret them to generate a construct of
the studied phenomenon 15. This construct resulted in three categories of analysis: Clinical complications
and feeding of premature children worry mothers after hospital discharge; Maternal
perception of the adequate development of the premature child, but in need of stimulation;
and Vulnerable situations generate concern, fear, and insecurity regarding home care.
The research was approved by the Research Ethics Committee (Reference n° 2.055.584
/ 2017, CAAE 66155417.6.0000.5393 - Resolution 466/2012). We used the STROBE Instrument
(Strengthening the Report of Observational Studies in Epidemiology) and COREQ (Consolidated
Criteria for Reporting Qualitative Research) to guide the methodology. This study
considered all the ethical standards of the 1973 Declaration of Helsinki, in addition
to complying with the principles of respect, autonomy, beneficence, and confidentiality
of information.
To collect data from medical records, a commitment to collecting data from files was
signed, in compliance with the personal data protection law. For the interviews, the
Free and Informed Consent Form was used, and the participants were identified by the
letter (P) "participant", with the sequential number of the interview, for example,
P1 (Participant 1) and so on. The meetings with the mothers were represented by an
HV 15 days after discharge, Phone Call I (Phone I) 30 days after HV, and Phone Call
II (Phone II) at six months of the chronological age.
Results
In the five-year period between 2013 and 2017, the prematurity rate was 10.3%, and
of these children, 43.3% (n = 951) needed to be hospitalized. More than 30% of newborns
were born weighing less than 1,500 g, as well as being extremely premature and or
very premature (<28 and between 28 and 31 weeks, respectively), which can lead to
greater vulnerability of these children to negative repercussions of their health
condition resulting from prematurity. Likewise, the conditions of clinical instability
in the first minute of life, that is, Apgar scores below seven, were present in more
than 30% of premature babies, thus demonstrating the potential for the appearance
of special health needs in the short and long term (Table 1). The length of hospital stay (greater than seven days) was considered to be a risk,
as the longer the stay, the greater the morbidities.
Table 1
Data on Premature Children Hospitalized between 2013 and 2017, Related to the Development
of Special Health Needs. Foz do Iguaçu, PR, Brazil, 2017/2018
|
Variable
|
n
|
%
|
p-value
|
|
Weight at birth
|
|
≤ 1,000g
|
143
|
15.0
|
|
|
1,001-1,500g
|
204
|
21.5
|
|
|
1,501-2,499g
|
506
|
53.2
|
<0.0001
|
|
2,500-3,999g
|
95
|
10.0
|
|
|
≥ 4,000g
|
03
|
0.3
|
|
|
Gestational age
|
|
< 28 weeks
|
126
|
13.2
|
|
|
28-31 weeks
|
233
|
24.5
|
<0.0001
|
|
32-33 weeks
|
280
|
29.5
|
|
|
34-36 weeks
|
312
|
32.8
|
|
|
Apgar 1st minute
|
|
< 7
|
349
|
36.7
|
|
|
≥ 7
|
596
|
62.7
|
<0.0001
|
|
Omission
|
06
|
0.6
|
|
|
Apgar 5th minute
|
|
< 7
|
104
|
10.9
|
|
|
≥ 7
|
841
|
88.5
|
<0.0001
|
|
Omission
|
06
|
0.6
|
|
|
Complications
|
|
Yes
|
658
|
69.2
|
<0.0001
|
|
No
|
293
|
30.8
|
|
|
Length of Hospital
|
|
< 7 days
|
221
|
23.2
|
<0.0001
|
|
7 days or more
|
730
|
76.8
|
|
The prolonged hospitalization time of premature children was correlated with lower
gestational age, low birth weight and a greater number of complications. In the same
way, the high number of complications with lower gestational age, low birth weight
and prolonged hospitalization (Table 2).
Table 2
Pearson Correlation between Length of Hospital Stay and Complications, and Gestational
Age, Birth Weight, Apgar Scores at 1st and 5th minute in Children Born Prematurely.
Foz do Iguazu, PR, Brazil, 2017/2018
|
Variable
|
n
|
R
|
IC 95%
|
p-value
|
|
Length of Hospital
|
|
Gestational age
|
951
|
-0.199
|
(-0.26; -0.14)
|
0.0000
|
|
Weight at birth
|
951
|
-0.302
|
(-0.36; -0.24)
|
0.0000
|
|
Apgar 1st minute
|
945
|
0.004
|
(-0.06; 0.07)
|
0.9010
|
|
Apgar 5th minute
|
945
|
0.048
|
(-0.02; 0.11)
|
0.1380
|
|
Complications (n)
|
951
|
0.499
|
(0.45; 0.55)
|
0.0000
|
|
Complications (n)
|
|
Gestational age
|
951
|
-0.2426
|
(-0.30; -0.18)
|
0.0001
|
|
Weight at birth
|
951
|
-0.2380
|
(-0.30; -0.18)
|
0.0001
|
|
Apgar 1st minute
|
945
|
-0.1527
|
(-0.21; 0.09)
|
0.0001
|
|
Apgar 5th minute
|
945
|
-0.0926
|
(-0.16; -0.03)
|
0.0050
|
Maternal Perceptions: Incorporating Quantitative and Qualitative Data
Clinical complications and feeding of premature children worry mothers after hospital
discharge
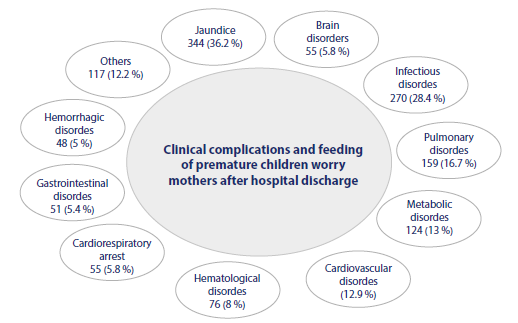
Jaundice and infectious, pulmonary, metabolic, and cardiovascular disorders were identified
as the most common complications during the hospitalization period and were confirmed
in maternal reports from the interviews (Figure 1).
Figure 1
Diagnosis/Complications of Children Born Prematurely and Hospitalized between 2013-2017,
and the Child's Complications during Hospitalization and Immediately after Hospital
Discharge, as Perceived by Mothers. Foz do Iguaçu, PR, Brazil, 2017/2018
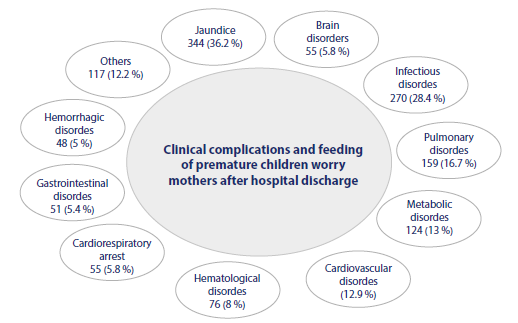
Source: elaborated by the authors.
The clinical complications that worried mothers were identified at the time of discharge
and after one month. Many of these complications occurred due to prematurity itself,
as well as to events inherent to the hospitalization period. Nutrition and its difficulties
described in the healthy growth and development of premature children were attributed
to the relationship between health and adequate weight gain in children.
She's gained more weight, she's stronger, she's smarter. She follows us with her eyes
a little, acts a little more in the morning and cries. (P2 - Phone I)She's breastfeeding,
I make her burp, she burps well. Then I spend a few minutes and she starts to get
irritated, squeezes herself [...]. They said that it may be reflux that is causing
it. (P18-HV) He needs to be monitored by the cardio pediatrician due to a complication
during the hospitalization period, endocarditis. (P13- Phone I) [... ] we had to come
back because of the inguinal hernia, and we stayed in the hospital for almost a week.
(P13-HV)
Maternal perception of the adequate development of the premature child, but in need
of stimulation
In the group of children followed up until six months of chronological age, it was
possible to identify that five of them were in the group of premature infants with
gestational age between 28 and 31 weeks; five children weighing less than 1,500g;
and 18 children remained hospitalized for more than seven days.
Figure 2
Scores of Developmental Milestones and Behavioral Symptoms (verified at six months
of age) Related to Gestational Age, Birth Weight, Length of Hospitalization and Maternal
Testimonies about the Development of the Premature Child. Foz do Iguaçu, PR, Brazil,
2017/2018
|
P |
GA |
BW |
Hospitalization |
SWYC |
BPSC |
Maternal perception of the adequate development of the premature child, but in need
of stimulation
|
|
01
|
32
|
1,265
|
43 days
|
14
|
01-04-00
|
I see that she is developing a lot, very hardworking, very smart. Depending on the
sound, she looks around with her little eyes. She pays attention. (P1-Phone I)
|
|
02
|
32
|
1,680
|
21 days
|
11
|
00-02-03
|
I think she is developing well, very slowly, that sometimes we don’t even notice.
(P2-HV)
|
|
03a
03b
|
33
33
|
1,920
1,790
|
24 days
21 days
|
11
11
|
02-03-02
00-05-04
|
The monitoring will be continuous, so I believe it will be alright. [...] maybe in
the future, they [twins] will need a speech therapist, neurologist, because they are
premature. So, I have these concerns. (P3-HV)
|
|
04ª
04b
|
31
31
|
1,715
1,390
|
17 days
34 days
|
19
19
|
01-07-02
01-07-02
|
They [twins] look at our faces and pay attention, they are doing well. (P4-HV)
|
|
05
|
31
|
1,685
|
28 days
|
10
|
02-02-02
|
She stays awake longer, especially during the day [...], she already laughs and when
I talk to her, she turns her head towards my voice. (P5-Phone I) Her neck is not firm,
then the doctor said we would observe her and, if necessary, refer to the physiotherapist.
(P5-Phone II)
|
|
06
|
30
|
1,190
|
47 days
|
13
|
00-00-00
|
He is developing fast, growing, getting fatter, watching things more, when I talk,
he looks for my voice, laughs a little. (P6-Phone I) He needs me to talk and play
with him a lot. (P6-Phone II)
|
|
07
|
32
|
1,915
|
11 days
|
16
|
00-00-00
|
He is smarter, when he listens, pays attention, fixes his eyes, I think he is developing
well. (P7-Phone I)
|
|
08
|
32
|
1,675
|
28 days
|
13
|
00-00-02
|
She is much smarter, more active, she knows my voice and that of her father, she wants
to sit on the lap, she interacts when I talk, she keeps her eyes fixed, looking for
the voice, laughs a little and tries to raise her head. (P8-Phone I)
|
|
09
|
33
|
1,720
|
21 days
|
08
|
00-04-02
|
He’s smarter, looking for the voice, interacting, paying attention when I talk to
him. He is very curious; he looks around the house. (P9-Phone I)
|
|
10
|
32
|
1,615
|
17 days
|
11
|
00-00-01
|
He still doesn’t try to lift his head and he doesn’t laugh. (P10-Phone I)
|
|
11
|
33
|
1,955
|
10 days
|
19
|
02-01-02
|
[...] gained weight very fast, she’s getting fat, who knows, so, as I’m telling you,
she’s developing well. (P11-HV)
|
|
12
|
34
|
2,840
|
6 days
|
12
|
00-02-00
|
[...] I think he is developing well. (P12-HV)
|
|
13
|
32
|
1,585
|
58 days
|
12
|
02-03-04
|
He is developing very well, and we are adapting. (P13-Phone I)
|
|
14
|
33
|
1,375
|
39 days
|
17
|
02-07-05
|
She already knows how to follow, she already knows how to stay upright, if I call
her from where I am she will direct her eyes. She is very smart; I think she is smarter
than she should be for her age. (P14-HV)
|
|
15
|
28
|
1,270
|
63 days
|
04
|
00-00-00
|
Normal, we don’t have another one to be able to compare, right? But up ‘till now everything
has been normal. (P15-HV)
|
|
16
|
34
|
1,585
|
5 days
|
15
|
02-00-00
|
She is developing well. She is much smarter, she pays close attention to everything
around her, when we talk to her, she looks for our voices, she laughs a lot. (P16-Phone
I)
|
|
17
|
34
|
1,810
|
8 days
|
17
|
02-02-01
|
He’s normal, he doesn’t even look like he was born premature. (P17-Phone I)
|
|
18
|
35
|
2,500
|
17 days
|
10
|
00-06-05
|
[…] I was afraid of him having some sequel. (P18-HV) She is paying more attention
when we talk to her, starting to laugh for the first time. (P18-Phone I) I need talk
and sing a lot with her. Yesterday I bought many books for her. (P18-Phone II)
|
From the SWYC score, it was found that eight children needed additional assessments,
meaning investigating the developmental milestones, as they had a score equal to or
below 11 on the scale. As for behavioral symptoms, according to the BPSC, ten children
needed professional evaluation, that is, they had subscales equal to or greater than
3.
Among the children with a low SWYC score, the majority were moderately premature infants
(32 and 33 weeks), with low weight (between 1,501g and 2,499g) and a hospitalization
period of more than seven days. For children with an unfavorable BPSC score, low weight
predominated, however, for most babies who were born with very low weight (1,001 and
1,500g), this score proved to be inadequate. Moreover, as in the SWYC, a long hospital
stay was a factor observed for babies with changes in the BPSC.
The testimonies revealed that most mothers do not identify delays in their child's
development, pointing out experienced moments such as laughter, curiosity, support
of the head, fixation of the gaze, looking for the voice, etc. However, some mothers
reported the need to adapt with a premature child at home, mentioning slowness in
growth and development and concerns for the long-term future.
I see that she is developing a lot, very hardworking, very smart. Depending on the
sound, she looks around with her little eyes. She pays attention. (P1-Phone I)
I think she is developing well, very slowly, that sometimes we don't even notice.
(P2-HV)
The monitoring will be continuous, so I believe it will be alright. [...] maybe in
the future, they [twins] will need a speech therapist, neurologist, because they are
premature. So, I have these concerns. (P3-HV)
Vulnerable situations generate concern, fear, and insecurity regarding home care
These circumstances of vulnerability result in insecurity and fear when caring at
home, especially due to the physical frailty presented by the premature baby.
I was a little afraid because she is so premature. I have never been a mother of a
premature baby, [...] what if something happens and I am alone. (P1-HV)
At the hospital we have all the help we need, any questions I had I could ask, but
here at home, I have to get by. (P2-HV)
The fears in exercising care and concerns about the child's future are added to the
maternal worries about their health, the susceptibility to catching diseases and the
need for further hospitalization.
Worry about her catching the flu. I'm worried about her health. (P7-HV)
You notice everything in the smallest details, out of fear. As there were many days
of hospitalization, you are very afraid to return. So, you have to take care of everything,
you know, always 100%. If you could put him in a bubble and leave him, in a bubble
you would leave him. (P13-HV)
[...] I am afraid that in the future something will happen. Because she is more fragile,
having a cold or something. (P18-HV)
The maternal notion from the recognition that premature children require more attention
and care leads to the identification of aspects of transformation and readaptation
of daily life.
I always keep an eye on her, you know? If she is breathing, if she is fine, if she
is awake [...]. (P5-HV)
It is living just for him [...]. Wow, after I had the baby, I didn't have time to
go to the salon, to go to the market, to take care of the house, anything, nothing,
just take care of him. (P6-HV)
Your attention is heightened due to the prematurity. (P3-Phone II)
Through the CSHN screening instrument, it was found, a priori, that mothers identified the special health needs of premature children, with greater
emphasis on the child's first six months of life, which involved the need for specialized
services and drug dependence.
Her neck is not quite strong enough. The pediatrician said that he would observe and,
when necessary, refer him to physiotherapy. The next day, he referred him to the physiotherapist.
(P5-Phone II) You need to go back to the cardiac pediatrician, neuropediatrician and
ophthalmologist, but so far, they've not called. And the infectologist too, because
of the syphilis test. (P8-Phone II)
You need to consult with a pediatric surgeon to get results from the herniorrhaphy.
With the cardio pediatrician and neuropediatrician to monitor complications during
hospitalization, he had seizures and endocarditis. (P13-Phone II)
She goes to the speech therapist for follow-up because she is premature, not that
she has had any problems. But she is taking domperidone because of reflux. (P18-Phone
II)
Regarding the recognition of children at risk of changes in development and behavior,
predictive factors for special health needs, identified in the quantitative stage,
were confirmed by the maternal concerns from the incorporation of the data.
Discussion
The findings of this investigation showed aspects that can enable the recognition
of the development of special health needs among premature newborns, such as low weight,
extreme and very preterm prematurity, Apgar scores below seven, complications during
hospitalization, and hospital stay longer. Mothers recognized that being born prematurely
may be a factor that predisposes their children to the need for further hospitalizations,
justified by the complications arising from the period in which they were initially
hospitalized. However, they believe that even in the face of prematurity, their children
have a healthy development, but they still express concerns about the child's health
and the need to reorganize family life.
The scientific literature indicates that the lower the birth weight and gestational
age, the greater the chances of prolonged hospitalization and short and long-term
health complications 7,16. These data were also identified by the correlation between gestational age, birth
weight, complications and length of hospitalization in this research. Extreme prematurity,
under 28 weeks, in a North American study was 6.4% 17, and in this investigation 13.2%, demonstrating its potential for the development
of special health needs 16. As well as this, among children followed up to the sixth month of life, moderate
preterm infants and those born with low weight were at risk of changes in development,
showing warning signs for specialized follow-up for children who remain hospitalized
for more than seven days.
Many babies did not have favorable Apgar score greater than seven, presumably due
to problems arising from the pregnancy, making them vulnerable to irreversible brain
damage, which may lead these children to death in the neonatal period, or to risks
of neurodevelopment problems in the long term 6,16,18.
By analyzing data from medical records and maternal testimonies, was observed that
the complications of hospitalization, such as jaundice, and infectious, respiratory,
metabolic, cardiovascular, hematological, and neurological disorders, resulted in
maternal concern, in which if the child was not well, may affect the relationship
and family life.
In particular, an extremely premature infant is more susceptible to serious complications,
which can even lead to death 16,19. Premature infants tend to develop pathological jaundice, which can result in complications,
such as cerebral palsy, affecting cognition and the sensorineural auditory system
5,16,19. These complications contribute to possible long-term special health needs, which
require specialized attention for these children 19. Complications of infectious origin, whether early (occurring within 48 hours) or
late (after 48 hours), are prevalent in the NICU due to several factors, such as baby's
weight, length of hospital stay, inadequate antibiotic therapy, among others, and
may lead to death, since early diagnosis is difficult, and the evolution of sepsis
can be rapid 7,20.
Respiratory complications are frequently reported with premature birth, especially
for children under 32 weeks, as this results from the immaturity of the premature
infant's respiratory system and consequent complications 16,17. A reality of this whole context is that mothers become insecure and, at times, overprotective
with childcare after hospital discharge because they have experienced hospitalization
and the appearance of complex complications.
Another relevant aspect is the change in family life, triggered by the understanding
of the fragility of the premature child, which can lead to suffering and make it difficult
to organize care. The international literature indicates that the perception of a
vulnerable parent can affect the adaptation and development of children with special
health needs and, therefore, it is essential to identify parental caregivers at risk
early to provide appropriate professional interventions 21.
By determining the SWYC score, it was found that in the follow up eight children out
of 20 needed additional assessments of developmental milestones, and ten for behavioral
symptoms, according to the BPSC.
The identification of risks and the correct intervention in early childhood are crucial
for the development of a healthy adult life 6,18. Mothers believe in the ideal development of their children, but they also express
concerns about the vulnerabilities caused by prematurity, which is common in the history
of children in this condition. In addition, complications during hospitalization can
occur, which must be treated early. Guidance for parental caregivers must be given
so that they can identify small delays in child development for intervention to be
performed 5,16. Therefore, it is essential to consider and understand the family context 22.
When considering the fragility of their children, mothers are afraid of the appearance
of diseases and further hospitalization. This corroborates with the concerns previously
mentioned, such as the research that followed preterm infants in the first year of
life and identified that 38% demanded further hospitalization 23.
Regarding the maternal identification of the demands of care presented by the child,
it is important to highlight that prematurity can have repercussions on long-term
factors of motor development, behavior, and cognition, and for this reason, it becomes
relevant to increase careful family orientation and assessment in all future consultations
19,24,25.
Health teams must provide adequate care support, through practices based on scientific
evidence 22,26,27, because families of premature infants with special health needs need to make available
an important amount of their time for the care of the child, and they require support
to readjust their daily life 19,28. Actions are needed for the insertion of parental caregivers into guidance and intervention
programs to encourage the neurodevelopment capabilities of premature children, in
the short- and long-term 12,18,22,29,30.
The study provides an understanding of the importance of considering birth and hospitalization
factors for special health care needs. This knowledge can provide support to carry
out the early stimulation of the premature and enhance healthy child development.
The bias of the text seems to be to emphasize the importance of early identification
of risk factors for special health needs, however, rapid identification and diagnosis
is necessary, so that children born prematurely have a better chance of survival and
quality of life, through more effective services.
Conclusion
The children who were born with low birth weight, extremely premature and/or very
premature, with Apgar scores below seven, who presented complications during hospitalization
and with a hospital stay longer than seven days, were recognized as children with
the potential to develop special health needs. These aspects were representative among
children with unfavorable scores in the SWYC and BPSC.
For mothers, their children showed healthy development, but they recognized that prematurity
and clinical complications from hospitalization are aspects of concern for the health
of their children, when considering the possibility of further hospitalizations, causing
maternal fear and insecurity for home care.
Thus, the results of this research are relevant and demonstrate the need for further
study on the subject to prevent and diagnose as early as possible physical and psychological
changes among children who show potential factors for developing special health needs.