The Perception of Nurses and Doctors on a Care Bundle Guideline for Management of Pain in Critical Care
Percepción de enfermeras y médicos sobre el uso de un paquete de atención como una guía para el manejo del dolor en cuidados críticos
A percepção das enfermeiras e dos médicos sobre o uso de um pacote de atendimento como guia para lidar com a dor em cuidados críticos
Recibido: 18 de abril de 2012
Enviado a pares: 4 de septiembre de 2012
Aceptado por pares: 29 de octubre de 2013
Aprobado: 9 de noviembre de 2013
Pathmawathi Subramanian1
Nick Allcock2
Veronica James3
Judith Lathlean4
1 Senior Lecturer, Department of Nursing Science, Faculty of Medicine, University of Malaya, Malaya.
pathmawathi@um.edu.my
2 Clinical Academic Professor of Nursing, Division of Nursing and Community Health, Glasgow Caledonian University, United Kingdom.
nick.allcock@nottingham.ac.uk
3 Professor Nursing Studies in the School of Nursing and Midwifery, University of Nottingham, United Kingdom.
veronica.james@nottingham.ac.uk
4 Professor of Health Research, University of Southampton, Faculty of Health Sciences, United Kingdom.
j.lathlean@soton.ac.uk
To reference this article / Para citar este artículo / Para citar este artigo
Subramanian, P., Allock, N., James, J., Lathlean, J. (2013). The Perception of Nurses and Doctors on a Care Bundle Guideline for Management of Pain in Critical Care. Aquichan. Vol. 13, No. 3, 336-346.
|
ABSTRACT Objective: The aim of this study was to explore nurses' and doctors' perception on using a care bundle as a guideline for the management of pain in critical care. Despite the development of evidence-based guidelines and protocols on the management of pain in critical care, pain is still a major problem. The introduction of care bundles in critical care has improved the management of ventilated patients. A care bundle in pain management aims to reduce variations in practice. Method: This study employed a qualitative prospective design using a semi-structured, in-depth interview of 23 nurses and doctors in a critical care unit. Result: Four main themes emerged: 1) suitability to the critical care setting; 2) applicability to the critical care setting; 3) ownership of the Pain Care Bundle; and 4) necessity for current practice. The results showed a poor uptake by the healthcare professionals in managing acute pain among critically ill patients. Conclusion: The study found that nurses and doctors did not perceive the pain care bundle as a useful tool for improving pain managment, with evidence pointing to a gap between pain management practice, as described by the care bundle, and actual practice. KEYWORDS Critical care, pain, pain management, nurses, perception, nursing. (Source: DeCS, BIREME). |
RESUMEN Objetivo: el objetivo de este estudio fue explorar la percepción de las enfermeras y los médicos sobre el uso de un paquete de atención como una guía para el manejo del dolor en cuidados críticos. A pesar del desarrollo de guías y protocolos para el manejo del dolor en cuidados críticos, basados en la evidencia, el dolor sigue siendo un problema importante. La introducción de un paquete de atención para cuidados críticos ha mejorado el manejo de los pacientes ventilados. Un paquete de atención en el manejo del dolor tiene como objetivo reducir las variaciones en la práctica. Método: el estudio tiene un diseño prospectivo cualitativo desarrollado mediante una entrevista en profundidad y semi-estructurada de 23 enfermeros y médicos en una unidad de cuidado crítico. Resultado: cuatro temas principales surgieron: 1) la adecuación al escenario de cuidado crítico, 2) la aplicabilidad al escenario de cuidado crítico, 3) la propiedad del Paquete de Atención al Dolor, y 4) la necesidad en la práctica actual. Los resultados mostraron una pobre aceptación del paquete por parte de los profesionales de la salud en el manejo de dolor agudo en los enfermos críticos. Conclusión: el estudio encontró que las enfermeras y los médicos no percibieron el paquete de atención al dolor como una herramienta útil para mejorar el manejo del dolor, con pruebas que apuntan a una brecha entre la práctica del manejo del dolor, tal como se describe por el paquete de atención, y la práctica real. PALABRAS CLAVE Cuidados críticos, dolor, manejo del dolor, enfermeras, percepción, enfermería. (Fuente: DeCS, BIREME). |
RESUMO Objetivo: o objetivo deste estudo foi explorar a percepção das enfermeiras e dos médicos sobre o uso de um pacote de atendimento como guia para lidar com a dor em cuidados críticos. Apesar do desenvolvimento de guias e protocolos para lidar com a dor em cuidados críticos, baseados na evidência, a dor continua sendo um problema importante. A introdução de um pacote de atendimento para cuidados críticos vem melhorando o tratamento dado a pacientes ventilados. Um pacote de atendimento no tratamento da dor tem como objetivo reduzir as variações na prática. Método: o estudo tem um desenho prospectivo qualitativo desenvolvido mediante uma entrevista em profundidade e semiestruturada de 23 enfermeiros e médicos em uma unidade de cuidado crítico. Resultado: quatro temas principais surgiram: 1) a adequação ao cenário de cuidado crítico; 2) a aplicabilidade ao cenário de cuidado crítico; 3) a propriedade do Pacote de Atendimento à Dor, e 4) a necessidade na prática atual. Os resultados mostraram uma baixa aceitação do pacote por parte dos profissionais em saúde no tratamento da dor aguda nos doentes críticos. Conclusão: o estudo constatou que as enfermeiras e os médicos não perceberam o pacote de atendimento à dor como uma ferramenta útil para melhorar o tratamento da dor, com provas que apontam a uma brecha entre a prática do tratamento da dor, tal como se descreve pelo pacote de atendimento, e a prática real. PALAVRAS-CHAVE Cuidados críticos, dor, manejo da dor, enfermeiras, percepção, enfermagem. (Fonte: DeCS, BIREME). |
Introducción
Various approaches have been used in health organizations to improve clinical outcomes (1), including clinical guidelines, protocols, practice policies, clinical policies, algorithms, standards and clinical pathways. (2) The development of the bundle concept is a new approach to ensure evidence-based practice to improve patient outcomes. (3)
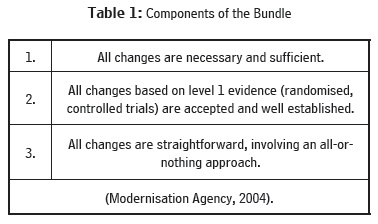
The concept of care bundles was developed in the United States in 2002. (4) A bundle is a collection of evidence-based interventions for the treatment of particular symptoms, which are used in combination. (5) A bundle is, therefore, a collection of three to five evidence-based interventions with components that, when performed together, should improve patient outcomes. Ventilator, sepsis, renal and nutrition care bundles have been developed. The Modernization Agency identified three core components to distinguish the care bundle from clinical guidelines and protocols (Table 1).
Following this, the National Institute for Clinical Excellence initiated use of the care bundle in critical settings in 2002, by developing new bundles through local service improvement groups. (6,7) The anticipated benefits of the pain care bundle (PCB) were improved pain management, improved utilisation of existing pain services, and a reduction in delayed discharge due to pain management problems.
The study was conducted in one adult critical care unit equipped with sixteen beds. The PCB components were developed to improve pain management practice, based on consensus ideas and expert opinion from the acute pain team. The components of the bundle also were based on a review of evidence from a range of sources, including The Royal College of Nursing, the Scottish Intercollegiate Guidelines Network, the Department of Health , the National Health Service, Quality Improvement Scotland and the Joint Commission on Accreditation of Healthcare Organisations. The PCB was divided into epidural (Table 2) and non-epidural PCB (Table 3). The epidural PCB has seven main components and is related to pain management for patients with epidural infusions, while the non-epidural PCB has five main elements.
Philosophical Assumption of the Study
In understanding the impact of the PCB on the development of effective pain management practices, it is important to identify nurses' and doctors' perception of the tool and to understand how it influences their pain management practices. Human beings involved in caring for others hold views or beliefs about the world, including what influences human behaviour and what constitutes quality of care. Clarification of these beliefs can assist in understanding the relationship between ontological and epis-temological issues. (8) The interpretive epistemology underlying this study provides valuable insights and exploration into human beings' meaningful actions, based on their pain guideline experience. and how to understand this action rationally. Interpretivist claim people's experiences are basically context-bound, (9) and researchers must understand the socially-constructed nature of the world and value its impact on the research process. (10) In terms of its theoretical foundation, the study was based on the Promoting Action on Research Implementation in Health Services model (PARIHS). (11-13) This model stresses that successful implementation occurs when the evidence is robust, the context is conducive and receptive to change, and where the change process is facilitated efficiently.
The Study
Aim
The aim of this study was to explore the factors that influence the uptake of a PCB among health care practitioners in a critical care setting. The primary focus of the study was to evaluate the usefulness and value of the pain care bundle in improving pain management.
Method
This study utilized a qualitative design with an interpretive approach to explore health care providers' perspectives on the context of the implementation of a pain care bundle and its influence on pain management.
Setting
The study was conducted in a large acute-care teaching hospital trust that provides a wide range of inpatient, outpatient, and day care services for a local population of more than half a million. The study was carried out in the adult critical care unit. It has an intensive care unit with seven beds, and a high dependency unit with ten beds.
Participants
A purposive sample of twenty three nurses and doctors participated in this study. This group was chosen to capture a rich description regarding their views on the PCB. Fifteen critical care nurses and eight doctors who were involved with patient management in the critical care unit took part in the study. The doctors were the key practitioners in planning care and managing the patients in the critical care setting, while the nurses were involved directly in the provision of care to critically ill patients in the adult critical care unit. The opinions and perceptions of key personnel are important in exploring the internal problems of any organisation. (14)
Ethical Consideration
The protocol and its subsequent amendments were developed in accordance with the ethical conduct of the research study based on the Declaration of Helsinki on vulnerable groups. The study also complied with the requirements of the Research Governance Framework for Health and Social Care, (2005). Formal ethical approval for the study was granted by the Local Research Ethics Committee and the Trusts' Research and Development Department. All the participants were given information about the study and assured of the confidentiality of the information they provided, and written consent was obtained from each participant prior to being interviewed.
Data Collection
A semi-structured, in-depth interview was chosen to explore the views of nurses and doctors about implementation of the PCBs, inasmuch as semi-structured, in-depth, open-ended interviews can provide valuable insight into the nature of phenomenon in naturalistic inquiry. (14) Data were collected over six months. The interview schedules provided prompt exploration the key issues related to the use of PCB and pain management practice. The interview guide was developed from key issues identified during the literature review (Table 4). The questions addressed issues pertaining to management of pain, the current approach to pain management, the strengths and limitations of current approaches to pain management, using the care bundle, and the challenges encountered in managing pain. Twenty three interviews were conducted with all participants consenting to the tape recording of their interviews. Each interview lasted 45 to 60 minutes.
Data Analysis
A total of 23 interviews were transcribed verbatim. Each interview was analysed using framework analysis, with the aid of the QSR NVivo 7 software program. Framework analysis was chosen because it is geared explicitly towards generating policy and practice-orientated findings. (15) In this study, the data collection and analysis processes were interwoven from the beginning. The framework analysis approach has five (5) key stages, which are:
Familiarization: Familiarization involves listening to the interview recordings and re-reading the transcripts until the researcher is familiar with the data.
Identifying a thematic framework: Here, the coding scheme identifies the key issues, concepts, and themes related to views about the PCB.
Indexing: In this case, the thematic framework was applied systematically to each transcript. Any interconnection of themes or multiple indexes was applied through charting, mapping and interpreting the association between the themes.
Charting: This involves rearranging the data according to the thematic content of each transcript and also by themes. Sub-themes for each participant were summarized using spreadsheets.
Mapping and Interpretation: This is the final stage of looking at the associations between themes and codes.
The key strategy involves the use of diagrams and tables to explore the relationship between the concepts and to define and illustrate the key concepts and the nature of the perceptions of the participants with regard to the PCB. Four main themes were subsequently developed. During the study, a journal was kept in which the contents and the process of interaction were noted, so as to increase self-awareness. The journal guided the researcher in keeping track of the relationships and provided material from reflection. By detailing decisions taken in the research process, a clear audit trail can be established to enhance dependability, fittingness and conformability.
Results
Participants
The participants' years of experience ranged from less than two (2) to more than 20, with the majority of participants having between two (2) and five (5) years of experience. Fourteen respondents were female and nine were male (Table 5).
Major Themes
Four major themes were identified: suitability, applicability, ownership and necessity. The participants' demographic details have been anonymised and changed to maintain confidentiality.
Suitability of the Care Bundle
The majority of the participants felt the PCB was not a useful guideline for pain management practice in the critical care unit. It was suggested the PCB components have limited alternative interventions to guide pain management, especially when pain management was perceived as difficult:
'...the PCB does not provide many alternatives (treatment). I think it is good for basic management, but for complex pain management or patients who cannot tolerate simple opiates, it is not suitable' (Doctor1).
Another participant noted the content of the PCB is very limited, since it states what the junior doctors and nurses should expect, rather than guiding an improvement in the patient's care. The respondents also indicated that some of the components of the PCB were only useful initially, such as paracetamol before the consideration of opioids. Most of the patients who were admitted to the critical care unit with acute pain following surgery were treated via an epidural catheter. Accordingly, the PCB was seen to be of limited relevance:
"... beyond pain scoring and paracetamol, giving analgesia and changing boluses, there is not awful a lot to do. I have to admit, there are not many interventions to carry out, whereas with the ventilator care bundle, there are a lot of aspects we have to deal with.' (Doctor2).
The care bundle was, therefore, seen by the participants to be of limited use, since it was regarded as recommending basic care, while failing to offer adequate alternatives, should basic care prove to be inadequate. Clinical leaders were not convinced that using the PCB improved pain management practices, since the scientific evidence was perceived as too limited to support practice. All good guidelines must embody the latest evidence-based practice to encourage consistent practice and to prevent clinical errors. (1) A study looking at why physicians do not follow clinical practice guidelines (16) suggested guidelines that do not indicate outcome measure may not work well in the clinical areas. The lack of clear, clinically measureable outcomes associated with pain management was seen as a limitation of the pain bundle.
Applicability to Pain Management
Fifteen participants, especially those involved with direct patient care, reported the PCB did not agree with the policy of the unit, which was developed within the Trust by staff members of the pain management team. Hence, there was a a perceived conflict between the unit's policy and the PCB. The participants explained this by comparing the differences in analgesia recommended in the PCB and the critical care unit.
'I agree all the components are evidence-based, but there is no evidence to support grouping them together like a bundle' (Nurse 1).
'I don't think the PCB addresses the needs of critically ill patients' (Nurse 2).
The participants, especially the nurses, felt the PCB was not applicable to critical care, since there was no evidence to show the bundle could improve practice, and that pain management for critical care patients is often complex and should be based on the individual patient's needs.
'I agree all the components are evidence-based but there is no evidence to support grouping them together like a bundle' (Doctor 3).
'For patients with significant morbidity to analgesia, particularly thoracic or upper GI (gastro intestinal), those who are at high risk of coughing, respiratory malfunction and breathing problems, we have a simple analgesia protocol, a complex analgesia protocol, and an almost separate epidural protocol. We are fairly free with how we mix and match. We have far more autonomy in our management plans. So, we don't quite fit in with the rest of the hospital and the ward management. I don't know if it fits in with the PCB or not, but that is what we often do it here. We don't have a fixed approach. We commonly use analgesia sedatives such as morphine, midazolam, propofol or alfentanyl for them' (Doctor 4).
Ownership of the Care Bundle
The participants explained the PCB was developed as a generic pain protocol and was not tailored to the needs of specific groups of patients. Since the PCB was developed by a regional network, it was created and intended to be applied to all the critical units in the region, and this was perceived as a weakness, making it less applicable to particular units:
'... the care bundle was developed over the network to cover six or seven different intensive care units, to cover a wide group of patient populations, and I don't think it is realistic to use in our unit, since we deal with a larger population and various types of cases' (Nurse 3).
Another participant gave similar examples; again, pointing out the PCB was perceived as an externally developed policy and, therefore, was not useful to this critical care unit, since every unit has its own organizational policies and procedures:
The problem with these guidelines is because they came from the network and are not meant for one hospital; and, different hospitals here use different drugs such as alfentanil and remifentanil. We can't put in specific guidelines, because each hospital has their own formula, different policy in purchasing and contracts. Even though it is a good framework, it does not meet everybody's needs' (Doctor 4).
Necessity for Current Practice
According to the participants, some of the components were similar to the Trusts' current pain management guidelines. Aspects of the recommendations in the bundle were seen as already being standard policy: for example, the use of paracetamol and opiates, and the components in the epidural care bundle. Therefore, it was felt the PCB added little to the current policy and, hence, provided little new understanding of possible approaches.
'... I have been practicing and it is not different from what we have been doing, it is actually recognized as good practice. I think we are good at it and don't necessarily follow the PCB, because it is within the practice' (Nurse 4).
The participants from all groups of professions felt that pain management is always handled well in the unit and there was no necessity for the introduction of a pain care bundle:
'I would say pain (management) is pretty good, and we are always aware when pain is an issue for patients. We don't need another pain guideline here.' [In the unit]. (Nurse 5).
The participants shared similar views on the generally good quality of pain management, and they also felt their pain management practice is good, as explained below:
'I think we are quite good at managing pain. The doctor, pain team and members of staff manage patients here well. We have more staff here and the doctors are more available compared to the [general] wards, and we have our consultant who knows what they are doing, and I think we are doing a good job here. We don't use the bundle to manage pain; we don't need it here' (Nurse 6).
Discussion
This study set out to explore nurses' and doctors' perceptions on the introduction of a PCB to improve pain management in critical care. The findings highlight a number of issues with regard to development and implementation of the PCB, which have affected its introduction and acceptance in the critical care setting studied. The findings highlight the importance of considering the three factors that are identified in the PARIHS framework when designing a practice improvement approach.
Despite that fact that care bundles have been shown to improve practice (17) and bundles relating to a number of aspects of critical care have been introduced, not to mention the existence of evidence suggesting room for improvement in relation to pain management, apparently there are several local contextual factors that have adversely affected development and introduction of the care bundle. The participants in this study appear to perceive current pain management as being good and, therefore, do not see the need for a PCB. The PCB was developed on a regional basis and this seems to have led to a lack of ownership and perceived conflicts with the local policy. There was a perceived lack of flexibility and also a lack of advice for more complex pain management issues. Interestingly, there also was a lack of perception of the benefit of combining interventions into a bundle in the field of pain and a perceived lack of evidence on which to base recommendations.
The nurses, in particular, wanted more guidance in advanced pain management. They needed guidance to assist their decisions beyond the administration of mild non-opiate analgesia and opiate analgesia, such as morphine. The lack of perceived benefit of the PCB over current policies also could have contributed to a perception that the PCB was not particularly useful in improving pain management. Moreover, the respondents concluded the PCB would be more useful if it was clearer and provided the more precise information needed to act as a reliable tool in managing pain.
When any guideline has been developed it needs to be appraised in terms of validity and reliability before being implemented. Guidelines of questionable validity could adversely affect patient care, be ineffective, or a waste of resources. (18) A good guideline needs to be identified by appraising the criteria set by the relevant accreditation bodies, such as the National Institute for Health and Clinical Excellence (NICE), and assessed by using tools such as the AGREE tool. However, developing the guideline is not in itself enough to ensure good implementation. As the PAHRIS framework suggests, context and facilitation are also important. Several aspects of the introduction of the PCB illustrated the difficulties that can be encountered, should these aspects not be adequately considered.
Implication for Nursing Practice
Prior to the completion of this study, there was no published research exploring the application and value of a PCB in the adult critical care population, using either qualitative or quantitative methodology. The findings suggest the development of a care bundle in pain management did not have a positive impact on self-reported pain management practices. While this study highlights the importance of considering all the factors identified in frameworks for introducing changes in practice, it also raises broader questions about the scope of the care bundle concept, which require further evaluation.
This study also illustrates the benefit of a qualitative evaluation of pain management practices among nurses. Qualitative evaluation was able to identify the percpetions of the health care staff introducing the PCB and key weaknesses in the implementation strategy, which may have been missed by quantitative evaluation of outcomes in, for example, an audit. This study was limited to one location and, therfore, can only provide limited insight. Further evaluation of the potential benefits of the PCB are needed before any firm conclusions about the benefit of a PCB can be reached.
Conclusion and Recommendations
This study highlighted a number of difficulties associated with the introduction of a PCB in a critical care unit in the UK. Although there were a number of aspects of the introduction of the PCB that might account for these difficulties, it also raises a question regarding the applicability of the care bundle concept. Further research is needed to assess the implementation of care bundles before their potential impact on pain management can be evaluated.
Bibliographic References
1. McMaster P, Rogers D, Kerr M, Spencer A. Getting guidelines to work in practice. Archives of Disease in Childhood. 2007;92:104-106.
2. Miller M, Kearney N. Guidelines for clinical practice: development, dissemination and implementation. International Journal of Nursing Studies. 2004;41(813-821).
3. National Health Service Modernisation Agency. 10 High Impact Changes for Service Improvement and Delivery: A Guide for NHS Leaders. 2004.
4. Berenholtz S, Dorman T, Ngo K, Provonost P. Qualitative review of intensive care unit quality indicators. Journal of Critical Care. 2002;17:12-15.
5. Fulbrook P, Mooney S. Care bundles in critical care: a practical approach to evidence-based practice. Nursing in Critical Care. 2003;8:249-255.
6. National Institute for Clinical Excellence. Principles for Best Practice in Clinical Audit. Oxford. 2002.
7. National Institute for Clinical Excellence. Progress Report on NHS Evidence. Special Health Authority;2008.
8. Benton T, Craib I. Philosophy of Social Science: The Philosophical Foundations of Social Thought. 1st ed. New York: Palgrave MacMillan; 2001.
9. Holloway I, Wheeler S. Qualitative Research for Nurses. 1st ed. London: Blackwell Science Ltd; 1996.
10. Denzin NK. The Research Act: A Theoretical Introduction to Sociological Methods. 3rd ed. Englewood Cliffs NJ: Prentice Hall; 1989.
11. Harvey A, Rycroft-Malone J, Titchen A, Kitson A, McCormack B, Seers K. Getting evidence into practice: the role and function of facilitation. Journal of Advanced Nursing. 2002;37(6):577-588.
12. Rogers E. Diffusion of Innovations. 4th ed. New York: Free Press; 1995.
13. Rycroft-Malone J, Seers K, Titchen A, Harvey G, Kitson A, McCormak B. What counts as evidence in evidence-based practice? Journal of Advanced Nursing. 2004;3(1):81-90.
14. Patton M. How to Use Qualitative Methods in Evaluation. 1st ed. London: Sage Publications; 2001.
15. Green J, Thorogood N. Qualitative Methods for Health Research. 1st ed. London: Sage Publications Limited; 2004.
16. Cabana M, Rand C, Powe N, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. Journal of American Medical Association. 1999;282:1458-1465.
17. Al-Tawfiq JA, Abed MS. Decreasing ventilator-associated pneumonia in adult Intensive care units using the institute for healthcare improvement bundle. American Journal of Infection Control. 2010;38(7):552-556.
18. Grol R, Grimshaw J. From best evidence to best practice: Effective implementation of change in patients' care. The Lancet. 2003;362:1225-1230.