Coping and Health Problems of Caregivers of Survivors with Traumatic Brain Injury
Afrontamiento y problemas de salud en los cuidadores de sobrevivientes con lesiones traumáticas del cerebro
Adaptação e problemas de saúde cuidadores de sobreviventes com lesões cerebrais traumáticas
Recibido: 2 de octubre de 2012
Enviado a pares: 2 de octubre de 2012
Aceptado por pares: 2 de septiembre de 2013
Aprobado: 1 de noviembre de 2013
DOI : 10.5294/aqui.2014.14.2.5
Prangtip Chayaput1
Ketsarin Utriyaprasit2
Somsong Bootcheewan3
Orapan Thosingha4
1 PhD. Assistant Professor, Mahidol University, Thailand.
prangtip.cha@mahidol.ac.tli
2 Assistant Professor Dr., Mahidol University, Thailand.
ketsarin.utr@mahidol.ac.th
3 MNS. Advanced Practice Nurse, Ayutthaya Hospital, Thailand.
s_bootcheewan@hotmail.com
4 DNS. Assistant Professor, Mahidol University, Thailand.
orapan.tho@mahidol.ac.th
Para citar este artículo / To reference this article / Para citar este artigo
Chayaput P, Utriyaprasit K, Bootcheewan S, Thosingha O. Coping and Health Problems of Caregivers of Survivors with Traumatic Brain Injury. Aquichan 2014; 14(2):170-183. DOI : 10.5294/aqui.2014.14.2.5
|
ABSTRACT Objectives: To evaluate coping and the health problems of caregivers at the time of survivor discharge and at one month after discharge and to determine correlations among personal data, coping and health problems of caregivers and disability of survivors. Method: Eighty-five dyads of survivors with traumatic brain injury and their caregivers were included. The instruments employed for data collection were the 27-item Thai version of the Coping and Adaptation Processing Scale-Short Form, the Health Problem Questionnaire for caregivers and the Disability Rating Scale for survivors. The Roy Adaptation Model was used as a conceptual framework for this study. Pearson's product moment correlation coefficient was employed for analysis. Results: No statistical differences were found between coping and health problems among caregivers. The health problems most frequently reported by caregivers were headache on the day of discharge and no health problems after one month of caregiving engagement. The disability level and marital status of the caregivers were correlated negatively with coping (r = -.245, p = .024, r = -.220, p = .043, respectively). Conclusions: The findings delineated that the caregivers remained able to handle the difficulties involved in caring for survivors at home with fewer health problems. Married caregivers were likely to manage this burden better than other caregivers. KEYWORDS Brain injuries, caregivers, adaptation, psychological, patient discharge, survivors, nursing (Source: DeCS, BIREME). |
RESUMEN Objetivos: Evaluar el afrontamiento y los problemas de salud de los cuidadores en el momento en que el sobreviviente fue dado de alta y un mes después de que el sobreviviente fue dado de alta. Además, determinar las correlaciones entre los datos de carácter personal, afrontamiento y los problemas de salud de los cuidadores y la incapacidad de los sobrevivientes. Método: Fueron incluidos en la investigación ochenta y cinco diadas de supervivientes con lesiones cerebrales traumáticas y sus cuidadores. Los instrumentos utilizados para la recolección de datos fueron la versión tailandesa de la Escala de Medición del Proceso de Afrontamiento y Adaptación - Formato Corto, con 27 ítems, el Cuestionario de Problemas de Salud para los cuidadores y la Clasificación de Escala de Discapacidad para los sobrevivientes. El Modelo de Adaptación de Roy se utilizó como marco conceptual para este estudio. La correlación producto-momento de Pearson se utilizó para el análisis. Resultados: No se encontraron diferencias estadísticas entre los problemas de afrontamiento y de salud en los cuidadores. Los problemas de salud reportados más frecuentemente por los cuidadores fueron dolor de cabeza en el día de alta y ningún problema de salud después de un mes de participación en el cuidado del sobreviviente. El nivel de la discapacidad de los sobrevivientes y el estado civil de los cuidadores se correlacionaron negativamente con el afrontamiento (r = - 0,245 , p = 0,024, r = - 0,220, p = 0,043, respectivamente). Conclusiones: Los resultados demuestran que los cuidadores permanecieron capaces de manejar las dificultades que implica el cuidado de los sobrevivientes en casa con menos problemas de salud. Los cuidadores casados eran propensos a manejar esta carga mejor que otros cuidadores. PALABRAS CLAVE Traumatismos encefálicos, cuidadores, adaptación psicológica, alta del paciente, sobrevivientes, enfermería (fuente: DeCS, BIREME). |
RESUMO Objetivos: avaliar a adaptação e os problemas de saúde dos cuidadores no momento em que o sobrevivente recebe alta e um mês depois disso, e determinar as correlações entre os dados de caráter pessoal, adaptação e os problemas de saúde dos cuidadores e a incapacidade dos sobreviventes. Método: 85 díades de sobreviventes com lesões cerebrais traumáticas e seus cuidadores foram incluídos na pesquisa. Os instrumentos utilizados para a coleta de dados foram a versão tailandesa da Escala de Medição do Processo de Enfretamento e Adaptação - formatação curta, com 27 itens, o Questionário de Problemas de Saúde para os cuidadores e a Classificação de Escala de Deficiência para os sobreviventes. O Modelo de Adaptação de Roy foi utilizado como marco conceitual para este estudo. A correlação produto-momento de Pearson foi utilizada para a análise. Resultados: não se constataram diferenças estatísticas entre os problemas de adaptação e de saúde nos cuidadores. Os problemas de saúde relatados mais frequentemente pelos cuidadores foram dor de cabeça no dia da alta e nenhum problema de saúde depois de um mês de participação no cuidado do sobrevivente. O nível da deficiência dos sobreviventes e o estado civil dos cuidadores se correlacionaram negativamente com o afrontamento (r = - 0,245 , p = 0,024 , r = -0,220 , p = 0,043 , respectivamente). Conclusões: os resultados demonstram que os cuidadores permaneceram capazes de lidar com as dificuldades que implica o cuidado dos sobreviventes em casa com menos problemas de saúde. Os cuidadores casados eram propensos a lidar com essa carga melhor que outros cuidadores. PALAVRAS-CHAVE Traumatismos encefálicos, cuidadores, adaptação psicológica, alta do paciente, sobreviventes, enfermagem (fonte: DeCS, BIREME). |
Introduction
The caregivers of disabled survivors with traumatic brain injury (TBI) are key persons in providing home-based care for those survivors. Nevertheless, before survivors are discharged from hospital, caregivers are given discharge instructions and preparation to offer care as part of routine nursing intervention (1).The impact of long-term responsibilities in caring for disabled survivors after they return to their rural homes, with limited support from local resources, is discussed thoroughly (2).
Survivors with traumatic brain injury are dependent on care-givers in the early stage following discharge from hospital, because neurobehavioral and/or physical deficits remain present even at 6-12 months post-injury (3,4). The caregivers of these survivors play a major role in fulfilling the demanding mission of facilitating recovery and rehabilitation (1,5).If the caregivers are unable to deal with this difficult situation, feelings of heavy burden, stress, anxiety and depression can occur, thereby leading to a decline in the status of their health (6,7).The aforementioned conditions affect functioning and caregiving ability (8).In turn, ineffective caregiving or inability to accomplish caregiving tasks can impact the patient's health status and disability rehabilitation (9).
As in the evidence from the aforementioned literature, the coping and health problems of caregivers are related to the rehabilitation of disabled survivors with TBI. These factors can promote or inhibit survivor rehabilitation.At the same time, the caregiver's health problems and ability to cope are categorized as a condition correlated with the disability of survivors with TBI during transition from the illness phase to the rehabilitation phase (10).
Several longitudinal follow-up studies (11-13) on survivors with TBI notea significant impact on caregiver roles.Several associations between caregiver quality of life, health status and survivor recovery also are evident in the findings of these studies. However, an evaluation of the difficulty in providing care for survivors with TBI during the immediate rehabilitation phase after discharge from hospital has been recommended (1,3).
Not many studies have been done to describe conditions related to the disability of survivors during the early rehabilitation phase (3), especially at one month after survivors are discharged from hospital and during continued home-based care. Following discharge from hospital, survivors continue to experience problems such as physical, cognitive and behavioral dysfunctions, which have both a personal and family impact (13,14).Caregiver ability to cope with accepting survivors' disability and re-adjusting to new roles is a crucial factor that influences the outcome of rehabilitation for survivors with TBI, as do the healthcare services and support required to help caregivers manage such problems in the long run (10,15).
The healthcare resources available to Thai survivors with TBI and their caregivers are unlike those in other countries where previously mentioned studies were conducted on the services and coverage offered. There are few studies on survivors with TBI and their caregivers in Thailand in the early stage following discharge from the hospital. Additionally, Thai culture and support in the duty of caring for ill family members with TBI remain vastly different from the situation in western countries (1,5).Thus, coping and the health problems of caregivers at the time of survivor discharge and at one month after discharge are examined in this study. Enhancing the understanding of coping and health problems among Thai caregivers in the early phase, with the support of increased evidence, can help to develop useful nursing interventions aimed at maximum restoration of caregivers' health and the recovery of survivors with TBI.
Therefore, the objectives of this study were:1) to evaluate the differences between the coping and health problems of caregivers upon the discharge of survivors with TBI and at one month after discharge; and 2) to determine the correlations among age, marital status, income, previous caregiving experience, coping, health problems of caregivers and the disability level of survivors with TBI.
Conceptual Framework
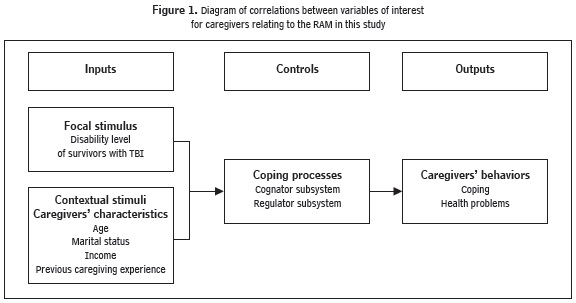
According to the Roy Adaptation Model (RAM), individuals -as adaptive bio-psychosocial systems - deal with challenging or threatening situations in their daily lives in order to survive (16). Changing environments or stressor persons perceived as posing difficulty act as stimuli. Focal stimulus refers to a stressor with direct influence on behavioral outcomes. Contextual stimuli are stressors that affect the focal stimulus, but also play a role in promoting behavioral responses (16-18).
Persons handle these stressors through cognator and regulator subsystems that function as an adaptive system to alleviate confronted stressors. A cognator subsystem is defined as a cognitive coping process, while a regulator subsystem is referred to as an automatic physiological process to maintain body system integrity (16).Persons perceive a threat or harmful stimulus that is provoked through a cognator, then moderate a regulator to stabilize the homeostasis of the body system (16,18).
In this study, the caregivers of survivors with TBI are adaptive individuals who were reacting to changing environments (1,18) and struggling with stressful experiences in the unpredictability of life situations by adjusting to the new role of being caregivers after returning home with the survivors. Thus, having a family member as a disabled survivor with TBI, i.e. the disability level of survivors, was a focal stimulus for the caregivers. The age, marital status, income and previous caregiving experience of the caregivers constituted the contextual stimuli.
Those factors contributed to effective or ineffective adjustment to the caregiving role through cognator and regulator subsystems. The abovementioned focal and contextual stimuli acted as inputs to manifestation of the caregivers' adaptation through relations to behavioral responses. The caregivers reacted and articulated through adaptive modes. Hence, the observed behavior; i.e. coping and health problems, pointed to the outcomes of the caregivers' nursing efforts or the outputs of the human adaptive system with respect to the RAM. If caregivers could adjust to their roles effectively, by completing essential daily living activities for survivors, the integrity of the caregivers' health status and family functioning could be maintained. On the contrary, any impediments to coping and caregiving activities could lead to a disruption of health and family integrity (1,16,18).
A diagram of the correlations between variables of interest to the caregivers in the present study with regard to the RAM (16) is provided in Figure 1.The conceptual-theoretical-empirical structure (19) of this study is outlined in Figure 2.
Materials and Methods
Participants
The sample size was calculated through the use of power analysis (20).To examine the differences between two measures by a correlated t-test and relationships, a two-tailed test with a power of .80, an alpha of .05, and a moderate effect size of .50 was set (21).According to this calculation, the minimum number of required participants was 85.
After the Institutional Review Board for Human Subjects had granted approval, 85 caregivers and 85 survivors with TBI living in rural areas were enrolled in this study subsequent to their discharge from four tertiary hospitals in the central region of Thailand. The caregivers of survivors with TBI who participated in the study were family members with no history of learning disability or psychiatric problems. They lived with the survivors and played a major role in taking care of them. The degree to which the survivors recruited for the study had to depend on the caregivers in daily living activities immediately after discharge from the hospitals was assessed using a Barthel Index of the Activities of Daily Living (BI) (22).All eligible survivors showed dependency on their caregivers for at least four out of ten activities, with scores under 10 on the BI.
All the participants were informed about the research objectives, methods, risks, benefits and ethical concerns with respect to confidentiality, anonymity and legal representation for granting permission for the incompetent survivors with TBI to take part in the study. Each of them also completed an informed consent form in writing.
Data Collection
Data were gathered using four instruments. Personal data on the caregivers; i.e. data on age, gender, marital status, education, income, employment, previous caregiving experience and relationship with survivors, were collected. The age, gender, marital status, education and employment of survivors with TBI were then recorded. The researcher collected the data by conducting a follow-up assessment on the coping and health problems of caregivers, as well as the disability level of survivors with TBI on the day of discharge and at one month after discharge. The ability of caregivers to cope was examined using the 27-item Thai version of the Coping and Adaptation Processing Scale-Short Form (23).Data on health problems were gathered using the health record form developed by the researchers. The disability level of the survivors with TBI was evaluated with the Disability Rating Scale (24,25).
Measurements
Thai Version of the Coping and Adaptation Processing Scale-Short Form
The 27-item Thai version of the Coping and Adaptation Processing Scale-Short Form (TCAPS-SF) was modified from the 47-item Thai version of the Coping and Adaptation Processing Scale (TCAPS), which was back-translated from the English version of Roy's Coping and Adaptation Processing Scale (CAPS) and validated (23). The CAPS was used to assess the coping strategy and based on the RAM and Roy's Nursing Model of Cognitive Processing (26).
The TCAPS-SF contains four subscales with 51.6% of the total explained variance:1) resourceful and systematic (eight items); 2) physical and fixed (six items); 3) positive and knowing (seven items) and 4) alert processing (six items).Most items denoted problem-solving coping strategies. Each item particularized the coping strategies individuals used to deal with difficult episodes confronted while maintaining a balance between work and routine daily activities (1,23,26).
The first subscale illustrates how individuals gather more information from any resource, think carefully step-by-step and develop strategies to overcome the problem at hand. The second subscale demonstrates how individuals react when faced with difficulty, e.g. overreaction, confusion and self-blame. The third sub-scale shows positive thinking and action toward solving problems. The last subscale represents how individuals take dynamic action to resolve problems (23).
The TCAPS-SF has good reliability (1,23). Cronbach's alpha coefficient for the total scale was 0.89 and ranged from 0.72 to 0.89 for each subscale (23).The following were used for the Likert-type four-level rating scale: 1 = never; 2 = rarely; 3 = sometimes and 4 = always. The total scores on the TCAPS-SF ranged from 27 to 108.Higher scores for each item illustrate more frequent use of specified coping strategies; i.e. the higher the score for each subscale, the more frequent the described coping strategy used by the individual (23).In this study, Cronbach's alpha coefficients for the total scale and each subscale were .79, .73, .75, .70 and .70, respectively.
Health Problem Questionnaire
The caregiver health problem questionnaire is a self-report checklist of possible health problems. It contains questions about what health problems caregivers faced at the time of survivor discharge from hospital and at one month after taking care of the survivor at home. The caregivers reported all health problems and rated the problems that concerned them the most. Two clinical nursing experts and a neurosurgeon examined the content validity of the questionnaire, which yielded a score of .90.
Disability Rating Scale
The 8-item Disability Rating Scale (DRS) was developed by Rappaport et al. (24) to measure the disability levels of patients with TBI. The scores ranged from 0 to 29.The minimum score of zero indicated no disability. Scores of seven to eleven illustrated moderately severe injury, and scores of 25 and above reflected an extreme vegetative state (24).The DRS had exhibited excellent reliability and validity for assessing the level of functional disability in populations with TBI (15,24,25).The inter-rater correlation among survivors with TBI in this study was one.
Data Analyses
Data analyses were conducted with a statistical computer package. The descriptive statistics used frequency, percentage, mean and standard deviation. A paired-samples t-test was performed to measure the differences between the coping and health problems of caregivers at the time of survivors' discharge and at one month after returning home. The correlations among the variables, including the disability level of survivors with TBI, age, marital status, income, previous caregiving experience, and the coping and health problems of caregivers, were calculated using Pearson's product moment correlation coefficient.
Results
Personal Data of Caregivers and Survivors with TBI
As shown in Table 1, the majority of the caregivers were married, employed, female and had primary educational achievements (Grades 1-6). Their ages ranged from 18 to 66, with the average being 40.85 years of age (SD 11.7).Most of the relationships with survivors were parental, followed by spousal or partner relationships with no caregiving experience.
The majority of the survivors with TBI were single, employed and male, and had high school educational achievements (Grades 7-12). Their ages ranged from 15 to 72, with the average being 29.59 years of age (SD 13).At one month after discharge, nearly all the survivors with TBI continued to show a dependency on caregivers for at least four out of ten activities on the BI. The BI scores were still under 10.
Coping and Health Problems of Caregivers
The mean coping ratings at the time of discharge and at one month after discharge were 81.88 (SD 9.22) and 83.45 (SD 7.83), respectively. There were no statistical differences between the total mean scores for coping and health problems among caregivers, as shown in Table 2.
With regard to the analysis of each coping strategy used, the caregivers applied similar strategies both at discharge and after having taken care of the survivors for one month. At one month after discharge, the caregivers indicated an increase in the coping strategies used for all of the items. Only one strategy was used significantly less; i.e. caregivers tended to blame themselves less for whatever difficulties they encountered after one month of performing caregiving tasks.
Table 3 illustrates the health problems mentioned most frequently by the caregivers; namely, headache, stress, no health problems, fatigue, backache and fever at the time of discharge. The health problems reported most often most at one month after discharge were no health problems, headache, fatigue, backache, stress and fever.
Disability Level of Survivors with TBI
The disability levels of the survivors with TBI averaged 4.41 (SD .82) on the day of discharge and 3.48 (SD 1.59)at one month after discharge. There was only one negative correlation between coping and disability level at the time of discharge (r = -.245, p = .024), as shown in Table 4. This study found no correlations among coping, health problems and disability level at one month after discharge, as illustrated in Table 5.
Relationships among Personal Data, Coping, Health Problems and Disability Level
The correlations among age, marital status, income, previous caregiving experience, coping, caregiver health problems and the disability level of survivors were sought. Only the marital status of caregivers was negatively related to the coping of caregivers (r = -.220, p= .043), as shown in Table 5. Furthermore, the married caregivers reported higher coping scores than the single, widowed and separated caregivers: 81.98 (SD 6.52), 81.34 (SD 9.84) on the day of discharge, and 83.72 (SD 6.88), 82.37 (SD 8.11) at one month after discharge. The married caregivers tended to make frequent use effective coping strategies after returning home. In other words, these findings suggest that married caregivers would be more likely to cope and to deal with the commitments involved in caring for disabled survivors effectively than single, widowed and separated caregivers.
Discussion
As for the personal data of the survivors with TBI, their characteristics are similar to those noted in other studies done in Thailand and western countries, with most of the survivors being young adult males (1,4,27).In Thai culture, caregiving and household responsibilities are usually the duty of the females in the family. Mothers, daughters, sisters and other female relatives are supposed to perform such tasks (1,28).Thus, most of the caregivers in the present study were found to be females and parents of survivors.
The survivors with TBI face major life-devastating impacts that distinguish them from healthy persons as they transition from the critically ill to the rehabilitation phase. Hence, caregivers play an important role in helping them to go through the abovementioned processes (1,5,6,9-11,15).Effective adjustment to these difficult consequences enables survivors to recover from disability, gain increased independence and improve their quality of life (27).
In terms of the coping strategies used by caregivers, it was found that they seek more resources and cope more effectively at one month after discharge, as the disability level of survivors gradually decreased. To the extent that the survivors with TBI began to recover, the fatigue, distress, and burden caregivers felt seemed to be alleviated (9), thereby enhancing the caregivers' satisfaction with their role. This study found the caregivers tended to blame themselves less after one month had passed. They were able to pursue caregiving roles effectively after feeling themselves able to facilitate the recovery of the survivors with TBI. For this reason, the ability of the caregiver to cope has direct impact on the survivor's recovery (14).
According to the RAM (16,18), it appears the caregivers coped with taking care of the survivors at home by accepting and adjusting to their new role. Subsequently, they were able to perform expected caregiving tasks and self-care with less dependency on others, eventually being able to return to work and to interact better with other members of society (18). They used more effective coping strategies by seeking resources, thinking carefully and being on the alert for new information about ways and means to care for the survivors effectively. According to the findings of this study, the married caregivers demonstrated adaptive behavior, reporting higher scores for coping and utilizing less emotional-solving coping strategies than single, widowed and separated caregivers.
For caregivers and family members, functioning was related significantly to the survivors' total scores for level of independence and disability (1,5,9).Moreover, in families with healthy caregivers who suffered no depression or sense of burden due to the demands of caregiving, the survivors with TBI had statistically significant higher levels of recovery from disability than in those with unhealthy caregivers. Caregiver health also resulted in good recovery of patients with TBI and enhanced survivor self-care ability (7).
How caregivers cope can adversely affect the status of their health (1,11,14,18).As for their health problems, emotional functioning, mental and physical health, many studies (29-32) clearly note correlations with the recovery outcomes of survivors with TBI in the rehabilitation phase. However, the caregivers in this study reported more problems with physical health than emotional functioning and mental health. This finding might be explained by the fact that Thai culture offers social support from families, friends and other resources in the community immediately after a survivor with TBI returns home (1,4,5,28). Consequently, the caregivers had taken advantage of all the obtainable support that was suitable for them (5).They might feel more positive and confident with less perceived role strain. Nonetheless, the decline in physical health was mentioned because the caregivers had to juggle new roles.
This study revealed that married caregivers deal with caregiving obligations better than single, widowed and separated caregivers. The findings also showed that most caregivers were parents and spouses. Other studies note reciprocal results in that caregivers who were parents (1) and spouses (1,33) also perceived caregiving responsibilities as less burdensome than adult-child caregivers. They had less difficulty adjusting to caregivers' lifestyles, because they accepted caregiving as a duty (1,5,28).In addition, the more the caregivers perceived the task as burdensome, the more likely they were to have mental health problems (14,31,33).Several studies (31,32,34) also have shown an increase in levels of depression and anxiety among both parental and spousal caregivers following the discharge of survivors with TBI. The aforementioned factors affected the success of the transition from hospital to home and placed the caregivers at risk of poor health-related quality of life and mental health problems.
The evidence-based findings in this study do not offer statistical support for correlations between coping and health problems at the time of discharge and at one month after discharge. However, the theoretical support from the RAM continues to show the context in terms of how the caregivers coped with the disability levels of survivors with TBI and how the health problems of the caregivers changed after they became involved with caregiving responsibilities.
Conclusion
In summary, the results explain how the caregivers of disabled persons with TBI were able to master the unexpected situations occurring in their lives during the acute rehabilitation phase at home. Caregivers' ability to cope with role adjustments in providing care for survivors with TBI was affected by several influential factors. The findings show caregivers were able to effectively handle the task of accompanying and caring for disabled survivors with TBI at home. The RAM can be engaged to describe the correlations between coping and the health problems of caregivers, as well as the disability levels of survivors.
However, further research to examine the proposed theoretical concepts is required. Nursing interventions to help caregivers continue to cope effectively should be established and implemented to meet caregivers' needs with accessible local resources. Even if the caregivers coped well with fewer health problems at one month after discharge from hospital, they would have a long-term duty to care for survivors with TBI who might recover slowly. Furthermore, most longitudinal studies have shown the long-term burdens involved in providing care for disabled survivors are correlated with the caregivers' quality of life. For this reason, followup studies are essential to improving the quality of nursing care among Thai caregivers and survivors with TBI.
Acknowledgement
This study was supported by the China Medical Board of New York, Inc. Mahidol University, Faculty of Nursing. It was present-ed during an oral session at the 10th Annual Conference of the Roy Adaptation Association (RAA), Boston College, Chestnut Hill, Massachusetts, USA.
References
1. Khiewchaum R, Thosingha O, Chayaput P, Utriyaprasit K. Coping with traumatic brain injury using the preparation program among caregivers of patients in the intensive care unit. Siriraj Med J 2011; 63(4): 128-31.
2. Hyder AA, Wunderlich CA, Puvanachandra P, Gururaj G, Kobusingye OC. The impact of traumatic brain injuries: A global perspective. Neuro Rehabilitation 2007; 22: 341-53.
3. Lippert-Gruner M, Kuchta J, Hellmich M, Klug N. Neurobehavioral deficits after traumatic brain injury. Brain Inj 2006; 20(6): 569-74.
4. Ta-ue I, Utriyaprasit K, Chayaput P, Sitthinamsuwan B. The relationships between post concussion syndrome and functional status in patients with mild traumatic brain injury. Thai J Nurs Council 2010; 25(2): 39-53.
5. Utriyaprasit K, Bootcheewan S, Chayaput P, Thosingha O. The relationship between social support to caregiver and patient's disability from traumatic brain injury. Siriraj Med J 2012; 64(6): 188-92.
6. Deeken JF, Taylor KL, Mangan P, Yabroff KR, Ingham JM. Care for the caregivers: A review of self-report instruments developed to measure the burden, needs, and quality of life of informal caregivers. J Pain Symptom Manage 2003; 26(4): 922-53.
7. Hart T, Millis S, Novack T, Englander J, Fidler-Sheppard R, Bell KR. The relationship between neuropsychologic function and level of caregiver supervision at 1 year after traumatic brain injury. Arch Phys Med Rehabil 2003; 84: 221-30.
8. Arango-Lasprilla JC, Plaza SL, Drew A, Romero JL, Pizarro JA, Francis K, et al. Family needs and psychosocial functioning of caregivers of individuals with spinal cord injury from Colombia, South Africa. NeuroRehabilitation 2010; 27: 83-93.
9. Sander AM, Carosell JS, High WM, Becker C, Neese L, Scheibel R. Relationship of family functioning to progress in a post-acute rehabilitation program following traumatic brain injury. Brain Inj 2002; 16(8): 649-57.
10. Watanabe Y, Shiel A, McLellan DL, Kurihara M, Hayashi K. The impact of traumatic brain injury on family members living with patients: A preliminary study in Japan and the UK. Disabil Rehabil 2001; 23(9): 370-8.
11. Blake H. Caregiver stress in traumatic brain injury. Int J Ther Rehabil 2008; 15(6): 263-71.
12. Lippert-Gruner M, Wedekind CH, Klug N. Functional and psychosocial outcome one year after brain injury and early onset rehabilitation therapy. J Rehabil Med 2002; 34: 211-4.
13. Livingston DH, Lavery RF, Mosenthal AC, Knudson MM, Lee S, Morabito DM. Recovery at one year following isolated traumatic brain injury: A western trauma association prospective multicenter trial. J Trauma 2005; 59: 1298-304.
14. Verhaeghe S, Defloor T, Grypdonck M. Stress and coping among families of patients with traumatic brain injury: A review of the literature. J Clin Nurs 2005; 14: 1004-12.
15. Hanks RA, Rapport LJ, Vangel S. Caregiving appraisal after traumatic brain injury: The effects of functional status, coping style, social support, and family functioning. NeuroRehabilitation 2007; 22: 43-52.
16. Roy C. The Roy adaptation model. 3rd ed. Upper Saddle River (NJ): Pearson Prentice Hall; 2009.
17. Chayaput P. Coping strategies of medical and surgical patients toward hospitalization: Roy Adaptation Model as a conceptual framework. Thai J Nurs Counc 2007; 22(2): 87-98.
18. Hanna DR, Roy C. Roy adaptation model and perspectives on the family. Nurs Sci Q 2001; 14(1): 9-13.
19. Fawcett J, Garity J. Evaluating research for evidence-based nursing practice. Philadelphia (PA): F.A. Davis; 2009.
20. Cohen J. A power primer. Psychol Bull 1992; 112: 115-59.
21. Munro BH. Statistical methods for health care research. 5th ed. Philadelphia (PA): Lippincott William & Wilkins; 2005.
22. Mahoney FI, Barthel D. Functional evaluation: The Barthel Index. Md State Med J 1965; 14: 56-61.
23. Chayaput P, Roy C. Psychometric testing of the Thai version of the coping and adaptation processing scale-short form (TCAPS-SF). Thai J Nurs Counc 2007; 22(3): 29-39.
24. Rappaport M, Hall KM, Hopkins K, Belleza T, Cope DN. Disability rating scale for severe head trauma: Coma to community. Arch Phys Med Rehabil 1982; 63(3): 118-23.
25. Wright J. The Disability Rating Scale. The Center for Outcome Measurement in Brain Injury. 2000 [ cited 2012 Aug 3 ]. Available from: URL: http://www.tbims.org/combi/drs
26. Roy C, Chayaput P. Coping and adaptation processing scale: English and Thai versions. RAA Rev 2004; 6(2): 4-6.
27. Duff D. Family impact and influence following severe traumatic brain injury. Axone 2006; 27: 9-23.
28. Potiprasat C, Sukonthasarn A, Sucamvang K. Caring behaviors and social support among caregivers of persons with head injuries. Nurs J 2005; 1: 1-13.
29. Sander AM, Maestas KL, Sherer M, Malec JF, Nakase-Richardson R. Relationship of caregiver and family functioning to participation outcomes after postacute rehabilitation for traumatic brain injury: A multicenter investigation. Arch Phys Med Rehabil 2012; 93(5): 842-8.
30. Arango-Lasprilla JC, Nicholls E, Villasenor Cabrera T, Drew A, Jimenez-Maldonado M, Martinez-Cortes ML. Health-related quality of life in caregivers of individuals with traumatic brain injury from Guadalajara, Mexico. J Rehabil Med 2011; 43(11): 983-6.
31. Ennis N, Rosenbloom BN, Canzian S, Topolovec-Vranic J. Depression and anxiety in parent versus spouse caregivers of adult patients with traumatic brain injury: A systematic review. Neuropsychol Rehabil 2013; 23(1): 1-18.
32. Nalder E, Fleming J, Foster M, Cornwell P, Shields C, Khan A. Identifying factors associated with perceived success in the transition from hospital to home after brain injury. J Head Trauma Rehabil 2012; 27(2): 143-53.
33. Conde-Sala JL, Garre-Olmo J, Turro-Garriga O, Vilalta-Franch J, Lopez-Pousa S. Differential features of burden between spouse and adult-child caregivers of patients with Alzheimer's disease: An exploratory comparative design. Int J Nurs Stud 2010; 47(10): 1262-73.
34. Turner B, Fleming J, Cornwell P, Haines T, Ownsworth T. Profiling early outcomes during the transition from hospital to home after brain injury. Brain Inj 2009; 23(1): 51-60.