Missed Nursing Care in Hospitalized Patients
Omisión en atención de enfermería para pacientes hospitalizados
Omissao no atendimento de enfermagem para pacientes hospitalizados
Recibido: 10 de octubre de 2014
Enviado a pares: 12 de octubre de 2014
Aceptado por pares: 14 de mayo de 2015
Aprobado: 19 de mayo de 2015
María Guadalupe Moreno-Monsiváis1
Catalina Moreno-Rodríguez2
María Guadalupe Interial-Guzmán3
1 Doctora en Filosofía, Universidad Autónoma de Nuevo León, México.
mgmoreno@hotmail.com
2 Magister en Ciencias de Enfermería, Hospital Christus Muguerza de Alta Especialidad, México.
catalina.moreno@christusmuguerza.com.mx
3 Magister en Ciencias de la Enfermería, Universidad Autónoma de Nuevo León, México.
mginterial@hotmail.com
Para citar este artículo / To reference this article / Para citar este artigo
Moreno-Monsiváis MG, Moreno-Rodríguez C, Interial-Guzmán MG. Missed Nursing Care in Hospitalized Patients. Aquichan. 2015; 15(3): 318-328. DOI: 10.5294/aqui.2015.15.3.2
|
ABSTRACT Objective: Determine missed nursing care in hospitalized patients and the factors related to missed care, according to the perception of the nursing staff and the patient. Method: Correlational descriptive study of a sample of 160 nurses and hospitalized patients, using the MISSCARE Nursing Survey. Results: Nursing personnel indicated there were fewer care omissions in continuous evaluation interventions (M = 94.56; SD = 11.10). The greatest number of omissions pertained to basic care interventions (M = 80.2; SD=19.40). Patients mentioned there were fewer omissions in continuous evaluation interventions (M = 96.32; SD=7.96), while the greatest number of omissions pertained to patient discharge and education (M=45.00; SD=23.22). The factors that contributed to missed nursing care, according to the nursing staff, were related to human resources (M = 80.67; SD=17.06) and material resources (M = 69.72; SD = 23.45); patients mentioned human resources and communication. Conclusions: Nursing care that is not carried out according to the needs of the patient, or is omitted or delayed, was identified. This aspect is relevant, since nursing care is fundamental to the recovery of hospitalized patients. KEYWORDS Nursing care, care, hospitalization, nursing staff, quality (Source: DeCS, BIREME). |
RESUMEN Objetivo: determinar el cuidado de enfermería no prestado a pacientes hospitalizados y los factores relacionados con la atención no prestada, según la percepción del personal de enfermería y la del paciente. Método: estudio descriptivo correlacional de una muestra de 160 enfermeras y pacientes hospitalizados, utilizando la Encuesta de Enfermería MISSCARE. Resultados: el personal de enfermería indicó que hubo menos omisiones de atención en intervenciones continuas de evaluación (M = 94,56; DE = 11,10). El mayor número de omisiones se refirió a intervenciones de atención básica (M = 80,2; DE = 19,40). Los pacientes mencionaron que hubo menos omisiones en intervenciones continuas de evaluación (M = 96,32; DE = 7,96), mientras que el mayor número de omisiones correspondió a dar de alta al paciente y a la educación (M = 45,00; DT = 23,22). Los factores que contribuyeron a la atención de enfermería no prestada, de acuerdo con el personal de enfermería, estuvieron relacionados con recursos humanos (M= 80,67; DE = 17,06) y recursos materiales (M = 69,72; DE = 23,45); los pacientes mencionaron los recursos humanos y la comunicación como factores determinantes en este sentido. Conclusiones: se identificó el cuidado de enfermería que no se lleva a cabo de acuerdo con las necesidades del paciente, o que se omite o retrasa. Este aspecto es relevante ya que la atención de enfermería es fundamental para la recuperación de los pacientes hospitalizados. PALABRAS CLAVE Cuidados de enfermería, atención, hospitalización, personal de enfermería, calidad (Fuente: DeCS, BIREME). |
RESUMO Objetivo: determinar o cuidado de enfermagem nao prestado a pacientes hospitalizados e os fatores relacionados com o atendimento nao prestado, segundo a percepqao da equipe de enfermagem e a do paciente. Método: estudo descritivo correlacional de uma amostra de 160 enfermeiras e pacientes hospitalizados, no qual se utilizou a Pesquisa MISSCARE. Resultados: a equipe de enfermagem indicou que houve menos omissoes de atendimento em intervenqoes continuas de avaliaqao (M = 94,56; DE = 11,10). O maior número de omissoes se referiu a intervenqoes de atendimento básico (M = 80,2; DE = 19,40). Os pacientes mencionaram que houve menos omissoes em intervenqoes continuas de avaliaqao (M = 96,32; DE = 7,96), enquanto o maior número de omissoes correspondeu a dar alta ao paciente e a educaqao (M = 45,00; DT = 23,22). Os fatores que contribuiram para o atendimento de enfermagem nao prestado, de acordo com a equipe de enfermagem, estiveram relacionados com recursos humanos (M= 80,67; DE = 17,06) e recursos materiais (M = 69,72; DE = 23,45); os pacientes mencionaram os recursos humanos e a comunicaqao como fatores determinantes nesse sentido. Conclusoes: identificou-se o cuidado de enfermagem que nao se realiza de acordo com as necessidades do paciente, que se omite ou atrasa. Esse aspecto é relevante já que a atenqao de enfermagem é fundamental para a recuperaqao dos pacientes hospitalizados. PALAVRAS CLAVE Cuidados de enfermagem, atendimento, hospitalizaqao, equipe de enfermagem, qualidade (Fonte: DeCs, BIREME). |
Introduction
In developed countries, an estimated one out of ten hospitalized patients suffers harm resulting from the care received or the omission of care; in developing countries, the proportion is much higher. According to the World Health Organization [WHO] (1), the most important aspect in terms of patient safety is to protect against harm during treatment related to care. Therefore, ensuring the quality of care and patient safety is the biggest challenge nurses and nursing leaders face today in managing care (2). Hence, the commitment of staff to provide quality nursing care commensurate with the treatment plan and to identify and meet each patient’s specific needs in a timely manner is fundamental.
Nursing care pertains to activities that are developed by the nursing staff, such as administering medication, patient ambulation , changes of position, bathing patients, mouth care, recording vital signs, intake and output documentation, nutrition, and education for hospital discharge, among others. When these essential elements of care are not offered to the patient, it is known as missed nursing care or errors of omission (3, 4). Previous studies show missed nursing care and errors of omission can be frequent at hospitals that attend to patients with acute health problems. According to WHO (1), an error is defined as the failure to complete a planned action, as intended, or the application of an incorrect plan. For example, an error can occur when something is done incorrectly (error of commission) or when something that should be done is not (error of omission). In the planning and implementation of care, regardless of whether the error is one of commission or omission, it is necessary to analyze why it occurred, to offer solutions, and to prevent any recurrence (3).
According to the Research Agency for Health Care and Quality, errors of omission are more difficult to recognize that errors of commission and, therefore, represent a major problem with serious implications for the quality and safety of care (5). The omission of nursing care can lead to adverse outcomes for patients, with significant harm, especially in vulnerable patient populations (6).
The phenomenon of missed nursing care was first identified by Kalisch (2) in a qualitative study designed to identify the types of nursing care that were regularly skipped during a hospital stay. According to the findings, Kalisch identified the major omissions in nursing care as being ambulation, position changes, mouth care, food tray delayed or not delivered, patient education, discharge planning, intake and output documentation, as well as hygiene and surveillance. Failure to comply with these elements of nursing care is attributed to lack of time, lack of staff for nursing interventions, poor teamwork, and ineffective delegation, among other factors. These findings were similar to those reported by Ball et al. (7).
Kalisch’s Missed Nursing Care Model (2) is the theoretical basis on which this study was based. Three concepts derived from the Model of Quality Care by Donabedian (8); namely, structure, process and outcome, are examined in this section. Structure refers to the infrastructure of the hospital, the patient care unit and the individual characteristics of nurses.
The process refers to nursing care given and nursing care or omitted care. The latter is regarded conceptually as an error by default and is defined as any aspect of required patient care that is omitted or delayed, all or in part (9). The result refers to the direct effects of nursing care on patient outcomes, such as falls, pressure ulcers and infections, and also on staff satisfaction with their current position and role.
According to this model, both the characteristics of the unit and the nursing staff have been linked to patient outcomes. Kalisch et al. (10) and Schubert et al. (11) indicate staff characteristics are associated with missed nursing care and impact on patient outcomes in the form of higher mortality rates, infection rates, pressure ulcers and falls. These complications, in many cases, result in longer hospital stays and higher costs for care, adding negative implications for the quality and safety of hospital care. The literature reports lower rates of missed care among nurses with professional status, higher levels of education, and more work experience, length of service and professional experience (10, 11, 12, 13, 14). As for the shift, missed nursing care has been found to occur more often during the night shift (7).
The Missed Nursing Care Model suggests there are factors that contribute to failure in care; the most common are attributed to human resources, material resources and communication. Regarding human resources, the focus is on staff profile (category, level of education, length of service, work experience, assigned service and shift), insufficient teamwork, ineffective delegation, staff shortages, high turnover, refusal to perform some care habits ("that is not my job" syndrome), the nursepatient relationship, poor use of human resources, and long working hours (15, 16, 17).
As for material resources, failure to provide the materials, equipment and supplies needed for care, and the availability of medical electrical equipment are two important factors. As for communication, the predominant factor is ineffective communication between support departments and the nursing and medical staff.
Identifying the type of missed or omitted nursing care and its associated factors is fundamental for nursing administrators; this knowledge allows for effective strategies that can contribute to the continuity of care. Another important aspect is that most studies, so far, have focused on errors of commission and have given little relevance to errors of omission, which are directly associated with the quality of care and the safety of the patient, as well as with health outcomes. Also, studies have focused on identifying the perception of nurses. The literature reports nurses are aware of the strengths and weaknesses in the care provided (18). However, there has been little emphasis on the opinions of the patient, who directly experiences the process of nursing care. Information from the patient is very useful and accurate, because it includes the result of an individual process of reflection on the care received from the nursing staff. Also, the patient may express his or her opinion according to the results of the attention received (19). Therefore, in the case of this study, it was considered important to identify the patient's perception as a recipient of care in order to contrast the perceptions of both (patient and nurse) about missed care. Consequently, the findings may provide evidence to design strategies that effectively help to reduce care omissions .
This study may contribute to the quality of nursing care by focusing on missed care, so as to design strategies to reduce care omissions. Likewise, it may provide nurses with knowledge by highlighting interventions that are not performed but are essential to patient recovery .
The following are the objectives of this study:
Identify missed nursing care during hospitalization, based on the perception of the nursing staff and the patient.
Identify missed nursing care according to the working characteristics of nurses (category, level of education, length of service, work experience and shift).
Determine the relationship between the perception of nurses and patients regarding missed nursing care.
Identify the factors whereby nursing care is missed during hospitalization, according to the perception of the nursing staff and the patient.
Method
The study design was descriptive and correlational (20). The study population was comprised of nurses and adult patients who were hospitalized at a private institution in the metropolitan area of Monterrey, Nuevo Leon, Mexico. Regarding the nurses, 160 participated out of a total census of 201 nurses assigned to inpatient service, where general surgery and internal medicine patients were being cared for. Nurses who were absent during the data collection period, for reasons of illness or vacation, were excluded; as were those who did not want to participate. Regarding the patients, 160 participated because they met the inclusion criteria: being conscious and situated in time and place, being 18 years of age or more, and having at least 48 hours of hospitalization. Once the 160 nurses were identified, one patient they had been assigned to serve was selected randomly. In situations where the patient had been selected previously, another was chosen randomly.
For collecting data on the nurses, the MISSCARE ("Missed Nursing Care") survey designed by Kalisch and Williams (21) was used. It consists of 64 items divided in three sections. The first section, with a total of 23 items, includes demographic and employment data on the nurses.
The second section, called "Missed Nursing Care," consists of 24 questions related to the elements of nursing care being provided to the patient. It is divided into four dimensions, including interventions to attend to individual needs, discharge planning and patient education, basic care interventions, and care interventions with continuous assessment. Response options are Likert-type and range from high to low: 5-always, 4-often, 3-occasionally, 2-rarely, 1-never and 0-does not apply. The "does not apply" option, was included in all the questions about nursing care that is not performed during the night shifts, such as feeding the patient and walking, among others. According to the authors, the answer choices are converted into a dichotomous scale; options 5 and 4 are regarded as care that was provide, while options 3, 2 and 1 are regarded as missed care. Cronbach's alpha obtained for this section was 0.89.
The third section, called "Reasons for Missed Nursing Care," consists of 17 items that pertain to the factors whereby nursing care is missed. It includes three dimensions for the factors involving human resources, material resources and communication. An Alpha value of 0.90 was reported for this section. The response rate is four-point Likert, where 4 denotes significant reason, 3 moderate reason, 2 minor reason and 1 is no reason.
The same MISSCARE survey (21) was applied to measure missed nursing care from the patient’s point of view. However, the questions from the first section were removed, because they were directly related to the job profile of nurses. This left only the patient identification data. The "Missed Nursing Care" section remained the same as was applied to the nursing staff, but care was taken to ensure the wording was consistent for the patient.
The section entitled "Reasons for Missed Nursing Care" was discarded for the patient application, because "do not know" was the dominant answer to the items in this section in the pilot survey. Therefore, the decision was made to formulate an open question: Why do you think nurses do not "always" provide some aspects of care? The final survey was composed of 33 items.
We asked permission from the authors (21) to use the survey and they allowed it to be translated for use in Mexico. Since the instrument had not been applied in the Mexican population, a translation process was necessary and the latest version underwent to a pilot study prior to being implemented.
For data collection, the hospital units were visited during each of the different shifts and the nursing staff was invited to participate. After the objective of the study had been explained, the staff members who agreed to participate were asked to sign an informed consent letter. After that, the staff members were asked if they wanted to answer the survey at that time; if they did, it was verified that doing so would not interfere with their planned activities. Then, the MISSCARE surveys were conducted. The participants received instructions on how to fill them out; likewise, they were told they were free to withdraw from the survey at any moment.
After that, a patient was selected randomly from those who were assigned to the nursing staff that had answered the survey previously and met the inclusion criteria. The authors visited the patients in their rooms to make sure they were experiencing no pain or discomfort and the survey would not interfere with any procedure. The study was explained to the patients and their participation was requested. Once the patients agreed to participate, each one was asked to sign an informed consent letter, then the authors proceeded to apply the MISSCARE survey to each patient. Moreover, it was verified beforehand that no staff member was in the room. This was done to obtain more openness in the patients’ responses. The study followed the ethical guidelines described in the Regulations for the General Law on Research in Health (22). In addition, the study was approved by the ethics and research committees of the Universidad de Nuevo Leon School of Nursing. Authorization from the participants was requested and obtained by having them sign an informed consent letter, and the dignity, privacy, welfare and rights of the patients were properly respected at all times.
The authors used the Statistical Package for the Social Sciences (SPSS),Version 17, to process the data. Descriptive statistics were used to profile the participants and to describe the variables of the study. Index values from 0 to 100 were designed for each of the dimensions of care, as well as for the associated factors. The higher the score, the more care given (the difference between the score obtained and the maximum possible amount is 100 for missed nursing care), and the more significant the reason for missed care. Inferential statistics, such as the Kruskal Wallis and Spearman correlation, also were applied to meet the objectives of the study.
Results
Nursing Staff Characteristics
The female gender predominated with 86.3%. The age range was 18-25 years (36.8%), followed by 41-50 years (20.7%), and the level of nursing education was Registered Nurse (53%) and Nursing Assistant (18.8 %).
As for job characteristics, more than half were in the RN category (or) BSN (61.9%), followed by Nursing Assistant (33.1%). The highest proportion had seniority with the institution and had been in its service from one to five years: 55.6% and 61.3%, respectively. Similarly, work experience was mainly one to five years (61.3%), and the swing shift dominated (41.2%), followed by the night shift (32.5%).
The average number of patients assigned to nurses per shift was six (SD = 4.24), admitted patients were three per shift (M = 2.94, SD = 1.48), and discharged patients were two (M = 2.01, SD = 1.60).
Patient Characteristics
The largest proportion of patients was served in the area of internal medicine (81.3%). As for gender, there was a slight predominance of women (55% female, 45% male). Regarding age, half of the participants were 51 or older; in relation to the level of education, over 50% had some degree of professional education and undergraduates predominated (46.3%).
Care Elements Perceived by the Nursing Staff
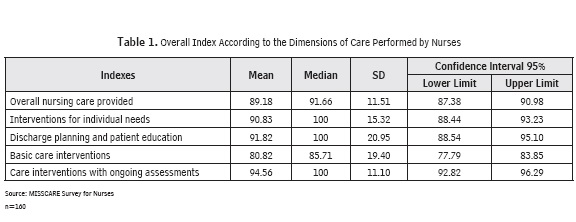
Table 1 shows the overall index and dimensions of the nursing care provided. The interventions that best pertain to fulfilled care-giving evaluations had an average of 94.56 (SD = 11.10), and basic care is where more missed or omitted care nursing was observed, at an average of 80.82 (SD = 19.40).
When analyzing the elements of missed care for each of the dimensions in terms of interventions to satisfy individual needs, the staff noted a higher proportion of missed or omitted care in the following order: emotional support for the patient and / or family (21.3%), assistance in attending evaluation visits for interdisciplinary care (14.7%), and drugs administered within 30 minutes before or after the scheduled time (11.1%).
As to discharge planning and patient education, care was perceived as missed by 5.7% with respect to patient education concerning the disease, testing and diagnostic studies, and 10.8%, in terms of the patient discharge plan and patient education. In basic care interventions, the attention that was found to have been missed most was assistance with ambulation three times per day or as ordered (42.0%), followed by feeding the patient while the food is hot (30.2%), and assistance with mouth care (21.3%).
Regarding care interventions with ongoing assessments, the main missed or omitted elements of care pertained to assessments and reassessments of patients per shift and health status: 13.5% and 12.8%, respectively.
Elements of Care Perceived by the Patient
Table 2 shows the rates of nursing care, according to the patient’s perception. The patient perceived greater compliance with interventions related to ongoing assessments, with an average of 96.32 (SD = 7.96). The dimension that showed more missed care was discharge planning and patient education, with an average of 45.0 (SD = 23.22).
By analyzing each of the dimensions, it was possible to identify the elements of care that were omitted most of the time. In the category of individual needs, the predominant missed or omitted care was emotional support for the patient and / or family (43.7%), followed by visits for assessments by other professionals (physician, nutritionist etc.),with 26.2%, and evaluating the effectiveness of drugs (16.7%).
In terms of interventions for discharge planning and patient education, patients reported shortcomings in education during hospitalization (about the disease, diagnostic tests and studies), as well as in the discharge plan: 36.2% and 73.7 %, respectively.
Regarding basic care interventions, missed care was higher in assistance for mouth care (32.1%), followed by assistance with hand washing (29.4%), ambulation three times daily or as ordered (20.3%), and support for changing position every two hours or according to the patient’s needs (17%).
Concerning activities for continuous assessment, the highest proportion of omission pertained to complete documentation of all required data on the patient (9.5%). Less omission was reported for this type of intervention .
Rates by nurses, according to their assigned category, level of education, length of service, work experience and assigned shift, were analyzed to identify differences in missed care according to the job characteristics of nursing care. Very similar values were obtained within each of the occupational characteristics . No statistically significant differences were found between groups when applying the Kruskal-Wallis test (p> 0.05).
The Spearman correlation test was applied to determine the relationship between the perception of nurses and patients about the care given and received. The results showed no significant association (p> .05).
Factors Related to Missed Nursing Care Perceived by Nurses
The factors where nursing care is missed or omitted, according to the perception of nurses, are shown in Table 3. Mainly, they are attributed to the nursing workforce, with an average of 80.67% (SD = 17.06), followed by materials and supplies, with an average of 69.72% (SD = 23.45), and, finally, communication factors, with an average of 65.16% (SD = 21.95).
Regarding human resources, the elements the nursing staff perceived as a significant reason for more than 50% of missed nursing care included an unexpected increase in the volume of patients (65%), followed by insufficient staff (58.8%), and patient emergencies (46.9%).
As for factors related to materials and supplies, nurses cited them as an important reason for missed care, specifically when drugs were not available (50%), followed by supplies / equipment not being on hand when needed, and supplies and equipment that do not work properly when required, with 36.9% and 33.8%, respectively.
Regarding the communication factors, unbalanced allocation of patients was perceived as the primary reason for missed care, with 40.6%, followed by too many tasks to be done for patients who are admitted and discharged, with 36.9%, and lack of support from team members, with 35.6%.
Factors Related to Missed Nursing Care Perceived by Patients
The patients noted that lack of staff is the main factor related to missed care (18.1%), followed by staff with insufficient experience (13.8%), and lack of organization and teamwork (7.5%). In a lesser proportion, they mentioned lack of staff communication from one shift to another (6.3%) and the attitude of staff members (5%), among other factors.
Discussion
There are elements of nursing care that are missed or omitted during a hospital stay, according to the perception of the nursing staff and patients. The dimensions where more nursing care is omitted, according to the perception of nurses, are related to basic care interventions, followed by interventions to satisfy individual needs. The patients agreed with the nursing staff about the omission of interventions to meet individual needs; however, they differed with the nurses by identifying a high degree of omission when it comes to discharge planning and patient education. The results regarding the omission of basic care interventions and those to satisfy individual needs were similar to the results reported by Kalisch et al. (3) and Kalisch and Lee (15).
The elements of nursing care omitted most often, as perceived by the nursing staff, were related to emotional support for the patient and / or family, attending evaluation visits for interdisciplinary care, and medication administered within 30 minutes before or after the scheduled time. Likewise, the patients agreed with the nursing staff in perceiving higher rates of omitted care in terms of emotional support for the patient and / or family, followed by attending evaluation visits with other professionals (doctor, nutritionist, etc.),and evaluating the effectiveness of medication. These results match those reported in studies by Kalisch (2) and Kalisch et al.(3).
As for discharge planning and patient education, both nurses and patients agreed these issues are missed continually during hospitalization. In addition, patients reported missed care for education about the disease, testing and diagnostic studies. These results coincide with those reported in studies by Kalisch et al. (3) and Kalisch and Lee (15). Consequently, these elements are important to emphasize. As pointed out by Kalisch (2) and Kalisch et al. (23), a lack of adequate patient education and little or no preparation for discharge has negative repercussions on patient outcomes, such as complications and readmissions.
Patient education is an important intervention that must be developed as a priority by the members of the nursing staff, because it helps them to improve their participation and to make informed decisions about care. On the other hand, the discharge plan ensures continuity of care and patient education during the hospital stay that is consistent with the patient’s specific needs. The goal, upon discharge, is to guarantee the patient and his/ her family can count on having adequate knowledge to manage treatment at home, if necessary (24).
As for basic care interventions, both the nurses and the patients perceived a significant proportion of missed or omitted care for assistance in walking three times a day or as ordered, followed by feeding the patient while the food is still hot, and mouth care. Also, the patients identified several aspects of missed care as being important, such as assistance in hand washing and support for position changes every two hours or as needed. These results agree with those reported by Kalisch et al. (3).
In general, basic care takes second place, since more priority is given to alternative care. Nurses assume basic care is done by the patients themselves, provided they have no physical or cognitive impairment and, if so, a family member would help. They considered routine nursing care in most hospitals as part of the care that must be performed by nurses and they take this opportunity to interact with the patient and to identify needs. Bittner and Gravlin (16) reported such care should be provided according to the category of nursing. The nursing assistant is responsible for routine care; however, the staff must make sure it is provided.
As for care that requires ongoing assessments, both nurses and patients perceived it as the type that is most likely to take place. However, both perceived omissions; the nurses said the care missed or omitted is that which includes the patient’s assessment of his/her health status. As for patients, they noted the care missed or omitted is that pertaining to full documentation of all required data. These findings are consistent with those of Kalisch et al. (3); they reported full documentation of the assessment of the patient in the nursing record sheet was one of the omitted / missed elements of care.
Some studies have found that missed nursing care, in the case of public hospitals, is associated with certain job characteristics of the nursing staff (5). However, this study discovered no differences in the care provided and missed according to those characteristics. This can be attributed to the fact that our study was performed at a private hospital, where a significant proportion of the nurses have less than 10 years of experience working with the institution and professional training predominates. Moreover, the participating institution has a continuing education program for nurses.
While both the nurses and the patients perceived missed or omitted care, there was no association between the perceptions of both groups. This might be because they perceived omission of care differently, based on the dimensions considered in this study; while the patients perceived more missed care regarding discharge planning and patient education, as well as interventions to satisfy individual needs; the nursing staff perceived it in terms of basic care interventions and interventions to meet individual needs. Most care omissions perceived by the patient are important to take into account. It is a priority for nursing to design strategies that allow for greater continuity of care in these key aspects, which are linked directly to the quality and safety of care provided to the patient during hospitalization.
Regarding the factors that might contribute to missed nursing care, the nurses mostly cited human resources, followed by material resources and communication. As for human resources, the predominant aspects were an unexpected increase in the volume of patients and not enough staff. The data in this respect are consistent with the results reported by Kalisch and Lee (15).
Having enough staff with specific skills is crucial to addressing the needs of patients. Whenever this aspect is affected, it directly interferes with the results of care, because nurses are forced to reduce or sometimes even skip certain tasks, even if doing so might increase the risk of adverse patient outcomes (11, 12 14).
Material resources were seen by the nurses as the second most important factor, especially when medicines and supplies / equipment are not available or might not work when needed. These results are similar to those reported by Kalisch et al. (3), Kalisch et al. (5) and Kalisch and Williams (21), who noted the proper functioning of equipment is necessary, as is its availability in the opportunity to provide quality nursing care and patient safety.
Regarding communication factors, the relevant aspects identified by the nursing staff focused on an unbalanced allocation of patients, the considerable amount of care required for patients who enter and leave, a lack of support from team members, and communication failures with the medical staff. These aspects identified in the study were similar to those reported by Schubert et al. (14) as ones that interfere with care. It is important to strengthen effective communication among all members of the health team at health-care institutions, because communication is one of the main elements that favors the continuity of care and helps to reduce care omissions through an adequate transfer of patient information.
Furthermore, it is important that subsequent studies on missed care and associated factors analyze the impact on patient outcomes, which is an aspect not considered in this study.
The findings of this study helped to identify, through the perception of nurses and patients, certain elements of care that are required, according to the patient’s specific needs, but not performed during hospitalization. They are omitted or delayed on occasion, which can affect the outcome of care. Moreover, in this study, the bulk of the omissions were those perceived by patients. This can be considered an important contribution, especially since the emphasis in previous studies was on identifying the perception of nurses.
Notably, both nurses and patients mentioned the factors related to human resources and ranked them first and foremost as being associated with missed care. All in all, this finding should be considered by nursing administrators as an area of opportunity that requires strategies to manage human resources effectively in an effort to reduce missed care and to strengthen the continuity of care.
References
1. Organización Mundial de la Salud. Marco conceptual de la clasificación internacional para la seguridad del paciente. Versión 1.1; 2009.
2. Kalisch B. Missed Nursing Care: A Qualitative Study. J Nurs Qual 2006; 21 (4): 306-313.
3. Kalisch B, Landstrom G, Williams R. Missed Nursing Care: Errors of Omission. Nurs Outlook 2009; 57 (1): 3-9.
4. Ausserhofer D, Zander B, Busse R, Schubert M, De Geest S, Rafferty AM, et ál. Prevalence, Patterns and Predictors of Nursing Care Left Undone in European Hospitals: Results from the Multi-country Cross-sectional RN4CAST Study. BMJ Qual Saf 2014; 23:126-135. doi:10.1136/bmjqs-2013-002318
5. Kalisch B, Tschannen D, Lee H, Friese C. Hospital Variation in Missed Nursing Care. AM J Med Qual 2011; 26 (4): 291-299.
6. Bittner NP, Gravlin G, Hansten R, Kalisch BJ. Unraveling Care Omissions. J Nurs Adm 2011; 41 (12): 510-512.
7. Ball JE, Murrells T, Rafferty AM, Morrow E, Griffiths P. "Care Left Undone" during Nursing Shifts: Associations with Workload and Perceived Quality of Care. BMJ Qual Saf 2014; 23: 116-125.
8. Donabedian A. Evaluating the Quality of Medical Care 1966. Milbank Q 2005; 83 (4): 691-729.
9. Kalisch B, Tschannen D, Lee KH. Missed Nursing Care, Staffing, and Patient Falls. Journal of Nursing Care Quality 2012; 27 (1): 6-12.
10. Kalisch B, Tschannen D, Lee KH. Do Staffing Levels Predict Missed Nursing Care? Int J Qual Health Care 2011; 23 (3): 302-308.
11. Ball J, Murrells T, Rafferty A, Morrow E, Griffiths P. "Care Left Undone" during Nursing Shifts: Associations with Workload and Perceived Quality of Care. BMJ Saf 2014; 23: 116-125.
12. Heede KV, Sermeus W, Diya L, Clarke SP, Lesaffre E, Vleugels A, et ál. Nurse Staffing and Patient Outcomes in Belgian Acute Hospitals: Cross-sectional Analysis of Administrative Data. International Journal of Nursing Studies 2009; 46: 928-939.
13. Kane R, Shamliyan T, Mueller Ch, Surval S, Wilt TJ. The Association of Registered Nurse Staffing Levels and Patient Outcomes. Medical Care 2007; 45(12): 1195-1204.
14. Schubert M, Glass T, Clarke S, Aiken L, Schaffert-Witvliet B, Sloane D, Gesst S. Rationing of Nursing Care and its Relationship to Patient Outcomes: The Swiss Extension of the International Hospital Outcomes Study. Int J Qual Health Care 2008; 20 (4): 227-237.
15. Kalisch B, Lee KH. The Impact of Teamwork on Missed Nursing Care. Nurs Outlook 2010; 58 (5): 233-241.
16. Bittner NP, Gravlin G. Critical Thinking, Delegation and Missed Care in Nursing Practice. J Nurs Adm 2009; 39 (3): 142-146.
17. Wakefield, B.J. (2014). Facing Up to the Reality of Missed Care. BMJ Qual Saf 2014; 23:92-94.
18. Moreno M, Interial G. Percepción del paciente acerca de su bienestar durante la hospitalización. Index Enferm 2012; 21(4), 185-189.
19. Ibarrola S, Beortegui E, Oroviogoicoechea C, Vázquez M. Evaluación de la satisfacción con los cuidados de enfermería en el área de hospitalización de cardiología. Enferm Cardiol 2011; XVIII(53), 27-33.
20. Grove SK, Burns N, Gray JR. Practice of Nursing Research. Appraisal, Synthesis, and Generation of Evidence. Elsevier St. Louis Missouri; 2013.
21. Kalisch B, Williams R. The Development and Psychometric Testing of a Tool to Measure Missed Nursing Care. J Nurs Adm 2009; 39 (5): 211-219.
22. Secretaría de Salubridad y Asistencia. Reglamento de la Ley General de Salud en Materia de Investigación para la Salud. México: Porrúa; 1987.
23. Kalisch B, Landstrom G, & Hinshaw AS. Missed Nursing Care: A Concept Analysis. Journal of Advanced Nursing 2009; 65(7), 1509-1517.
24. Consejo de Salubridad General. Estándares para Certificar Hospitales. Version 2012. México; 2012.