Article
Yeow Chye Ng1
Angela Caires2
1 orcid.org/0000-0003-3955-0440. College of Nursing, University of Alabama in Huntsville. United States. YeowChye.Ng@uah.edu
2 orcid.org/0000-0001-7030-0680. College of Nursing, University of Alabama in Huntsville. United States. Angela.Caires@uah.edu
Recibido: 11 de septiembre de 2016
Enviado a pares: 18 de septiembre de 2016
Aceptado por pares: 18 de octubre de 2016
Aprobado: 26 de octubre de 2016
Para citar este artículo / To reference this article / Para citar este artigo
Ng YC, Caires A. The Health Promotion Model in HIV Care. Aquichan. 2016; 16 (4): 418-429. Doi: 10.5294/aqui.2016.16.4.2
|
ABSTRACT Effective medical treatment with uninterrupted engagement in care is critical to improving the survival and the quality of life of patients infected with the human immunodeficiency virus (HIV). Objectives: Multiple behavioral interventions have been conducted to promote adherence behaviors. However, adherence to HIV medications and medical appointments is still an issue of global concern. Method: The Health Promotion Model (HPM) is a nursing adaption of the health belief model. The HPM focuses on individual characteristics and experiences, as well as behavior specific cognitions and outcomes. Integrating the HPM in addressing adherence behaviors could be one of the building blocks of success in changing health behavior. Results: A search of the literature turned up no studies that applied the HPM in adherence behavior studies conducted among HIV-infected populations. Conclusion: This paper presents the reader with the availability of current adherence-behavior interventions and strategies that align with the HPM model components. It further proposes the need for medical treatment team members to adopt the HPM in current clinical practice settings so as to effectively address adherence behavior issues. KEYWORDS: HIV medication adherence; adherence theory; health promotion model; linkage to HIV care; nursing promotion model (Source: DeCS, BIREME). |
RESUMEN Un tratamiento médico eficaz con un compromiso ininterrumpido en el cuidado es crítico para mejorar la supervivencia y la calidad de vida de los pacientes infectados con el virus de la inmunodeficiencia humana (VIH). Objetivos: se han llevado a cabo múltiples intervenciones conductuales para promover comportamientos de adherencia. Sin embargo, la adhesión a los medicamentos contra el VIH y las citas médicas siguen siendo un tema de preocupación mundial. Método: el modelo de promoción de la salud (HPM) es una adaptación de enfermería del modelo de creencias de salud. El HPM se centra en características y experiencias individuales, así como cogniciones y resultados específicos del comportamiento. La integración del HPM en el abordaje de los comportamientos de adherencia podría ser uno de los pilares del éxito en el cambio del comportamiento de la salud. Resultados: una búsqueda en la literatura no mostró ningún estudio que aplicó el HPM en los estudios de comportamiento de adherencia realizados entre las poblaciones infectadas por el VIH. Conclusión: este artículo presenta al lector la disponibilidad de las actuales intervenciones de adherencia-comportamiento y estrategias que se alinean con los componentes del modelo HPM. Además, propone la necesidad de que los miembros del equipo de tratamiento médico adopten el HPM en la práctica clínica actual con el fin de abordar eficazmente los problemas de comportamiento de adherencia. PALABRAS CLAVE: Adhesión a los medicamentos para el VIH; teoría de la adherencia; modelo de promoción de la salud; vinculación a la atención del VIH; modelo de promoción de la enfermería (Fuente: DeCs, Bireme). |
RESUMO Um tratamento médico eficaz com um compromisso ininterrupto no cuidado é fundamental para melhorar a sobrevivência e a qualidade de vida dos pacientes infectados com o vírus da imunodeficiência humana (HIV). Objetivos: realizaram-se múltiplas intervenções comportamentais para promover condutas de adesão. No entanto, a adesão aos medicamentos contra o HIV e às consultas médicas continua sendo um tema de preocupação mundial. Método: o Modelo de Promoção da Saúde (HPM, por sua sigla em inglês) é uma adaptação de enfermagem do modelo de crenças em saúde. O HPM centra-se em características e experiências individuais, bem como cognições e resultados específicos do comportamento. A integração do HPM na abordagem dos comportamentos de adesão poderia ser um dos pilares do sucesso na mudança do comportamento da saúde. Resultados: uma busca na literatura não mostrou nenhum estudo que aplicou o HPM nos estudos de comportamento de adesão realizados entre as populações infectadas pelo HIV. Conclusão: este artigo apresenta ao leitor a disponibilidade das atuais intervenções de adesão-comportamento e estratégias que se alinham com os componentes do modelo HPM. Além disso, propõe a necessidade de que os membros da equipe de tratamento médico adotem o HPM na prática clínica atual ao fim fim de abordar eficazmente os problemas de comportamento de adesão. PALAVRAS-CHAVE: Adesão aos medicamentos para o HIV; modelo de promoção da enfermagem; modelo de promoção da saúde; teoria da adesão; vinculação ao atendimento do HIV (Fonte: DeCs, Bireme). |
Introduction
The advancement of antiretroviral therapy (ART) has provided multiple positive health benefits to the HIV-infected population. The life expectancy of HIV-infected patients who choose to follow ART treatment has been dramatically prolonged. HIV is no longer considered a terminal illness by many medical professionals, but rather a chronic disease. However, many infected persons do not fully benefit from the best-managed treatment plans, because they do not consistently adhere to routine clinical care. Ensuring treatment adherence has proven to be a significant challenge in health care globally and in the United States.
Adherence is defined as the extent to which a patient follows instructions for prescribed treatment(s) (1) Individuals who do not fully adhere to prescribed treatment regimens may face higher mortality and morbidity rates due to the untreated advancement of their disease (2). Research has shown that effective medical treatment and correct diagnosis have proven to be critical to improving the quality of life of HIV patients and assuring their long-term survival (3). Failure to follow the precise recommendations and instructions of health care providers is a barrier to effective medical treatment. In addition, non-compliance or non-adherence to HIV care and treatment poses a significant economic burden to society (4).
Globally, non-adherence to antiretroviral therapy in the adult HIV-infected population ranges from 33% to 88 % (5). In the United States alone, non-adherence has led to tremendous yearly medical expenditures (6). In 2015, the global health observatory data repository indicated that approximately 1.1 million people died of HIV-related illnesses (7). The economic burden and death rate among HIV patients can be addressed and improved only through effective communication and commitment to the development and implementation of effective, evidence-based treatment regimens and adherence to them. Effective HIV treatment often requires a multidisciplinary team approach, and the coordination of care is critical to achieving success with respect to improving rates of adherence. Researchers have been struggling with the issue of adherence behavior for more than 50 years (8), and the problem of non-adherence is still listed as a priority research topic by the World Health Organization (9).
An extensive review of the literature uncovered no studies that developed and implemented the HPM as a methodology to address non-adherence behaviors. This paper discusses the clinical adherence intervention strategies currently available and explores other theoretical models that could successfully align with the HPM. In most clinical settings, nurses are the healthcare professionals who spend the most time with patients (10). Therefore, this is an opportunity for nurses to embrace the Health Promotion Model (HPM) to further encourage adherence behavior strategies among their patients.
The Health Promotion Model
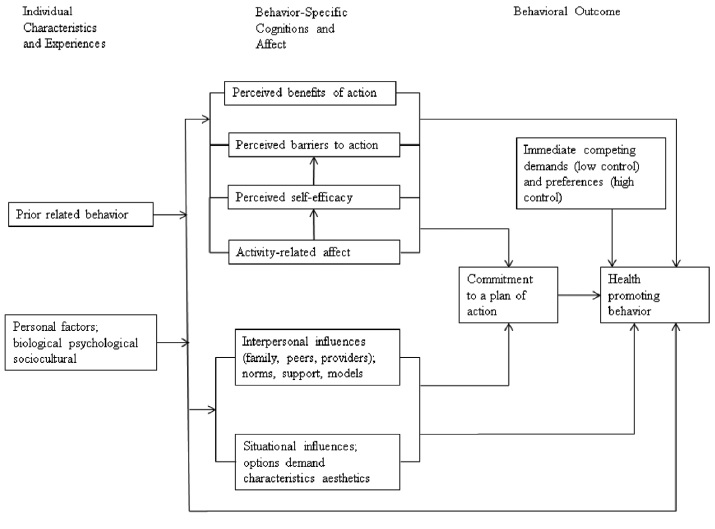
The Health Promotion Model (HPM) was designed as a health protection model that defined health as a state of positive metabolic and functional efficiency of the body and not merely the absence of disease The HPM is a nursing adaption of the health belief model, which is directed toward increasing a patient's level of well-being and self-efficacy as the patient interacts with the surrounding environment. Thus, the HPM is described as the art and science of assisting patients as they adapt to changes and improve their life style, while progressing toward a state of optimum health. Figure 1 provides an overview of the HPM, which focuses on three major components: 1) individual characteristics and experiences, 2) behavior-specific cognitions and affect, and 3) behavioral outcomes. The model maintains that each individual has personal experiences and characteristics that are unique to that person and can affect subsequent actions and outcomes (11). The behavior-specific knowledge variables have motivation characteristics that are helpful to improving individual engagement in health. These behavior variables can be applied in nursing. Thus, health promotion behaviors shape the desired behavioral outcome. Behavior should positively enhance a better quality of life, as well as improve functional abilities and health across all development stages.
The HPM embodies the following assumptions (11).
Patients must actively regulate their behavior.
Patients, in their biopsychosocial complexity, transform the environment as they interact progressively and transform behavior over time.
Physicians and nurses play an integral role in development of the interpersonal environment that exerts influence on the lives of patients.
Personal-environmental interactive patterns alter a patient's behavior.
Figure 1. Health Promotion Model (Adapted from 11)
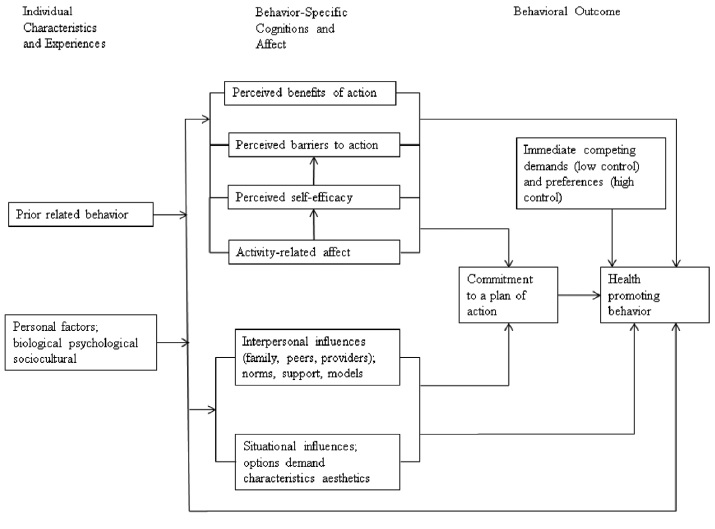
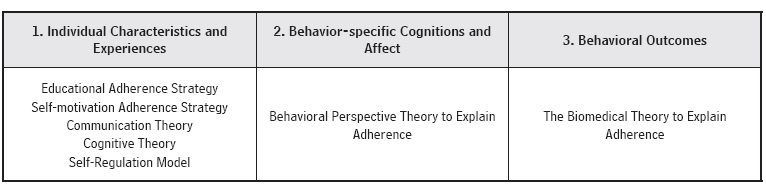
Table 1. The Relationship of Other Theories and Models with the Three Components of the HPM
Improving HIV Patient Adherence Using the HPM
HIV treatment effectiveness is based on the level of patient adherence to the therapeutic regimen. Health care systems, HIV-treatment team members, and patients all have a responsibility in improving adherence to medication. A single technique is not able to improve the adherence of HIV patients to a therapeutic regimen. Instead, the development and implementation of diverse methods focused on improving adherence is needed. Table 1 presents the different theories and models that have been applied to explore adherence behaviors. These theories and models are grouped under the three major components of the HPM: Individual Characteristics and Experiences, Behavior-specific Cognitions and Affect, and Behavioral Outcomes. These models could be implemented within the HPM framework by team members, with the overarching goal of improving adherence to scheduled medical appointments and daily medications.
1. Individual Characteristics and Experiences
Individual characteristics and experiences involve personal biological factors, psychological factors, and socio-cultural factors (12). The factors are shaped by the nature of the behavior in question and are considered to be predictive of a particular behavior(12). The following strategies could be implemented by treatment team members utilizing the HPM model:
The Educational Adherence Strategy
Most research supports the effectiveness of patient education in the areas of adherence, knowledge, and patient outcomes (6,13,14). Education positively impacts adherence among HIV patients, especially with regard to daily medication routines. This may be due to the many educational programs that are available to assist with improving adherence to treatment regimens. One example involves providing precise instructions and recommendations on self-care activities during scheduled medical appointments. Through collaborative care, adherence interventions can be implemented by utilizing the expertise of other treatment team members (physicians, nurses, dietitians, and social workers) (15). Nurses play a major role, not only in utilizing this strategy in daily practice, but also as team leaders who are pivotal in promoting collaborative care.
The Self-motivation Adherence Strategy
Koenig, Bernard (16) reported that adherence to a treatment plan improves as physicians use the patient's current laboratory results as a launching point in talking with the patient during clinical visits. As patients are made aware oftheir current viral load, this information may motivate them to take control of managing their health (16). Other interventions such as providing groceries, meal tickets, and other tangible bonuses as part of attendance rewards have been shown to improve adherence in routine HIV medical care (17,18). Directly observed therapy (DOT) is another strategy that also could improve medication adherence. Berg and colleagues conducted a randomized trial using DOT to explore adherence behavior. The study indicated DOT enabled patients to maintain low viral loads and found they were more accepting of future medical evaluations and more likely to maintain ART adherence (17).
Theoretical Models to Explain Educational and Self-Motivation Adherence
Educational and self-motivation adherence strategies are referred to as responses that are intended to improve an individual's ability to manage his/her disease(19). Behavioral principles such as feedback and reinforcement are often integrated into these strategies (19). The effectiveness of educational and self-motivational interventions should be tailored to address specific patient needs. Another important component that requires exploration is the quality of the relationship between the patient and the healthcare provider (20). The concept of educating patients and addressing their needs appears to be daunting and complex, and does not refer to didactic or cognitive theoretical models. Multiple theories (self-regulation perspectives, cognitive perspectives, and communication perspectives) can be applied to the socio-cultural and psychological factors in educating patients as they apply this knowledge and become self-motivated and more likely to adhere to their scheduled medical appointments and daily medication routines.
The Communication Theory
Communication models are essential to applying the educational and self-motivation strategies. These models focus on the transfer of knowledge and information related to a disease and its effective management (21). Communication models incorporate patient-specific information that can have a positive impact on motivation, as well as attitudes toward adherence.
Based on recent studies, it was found that information presented to patients should be tailored to a sixth grade reading level if it is to be effective and understood (22). Limiting prescribed messages to no more than three specific points, with supporting statements for each topic, was found to be most useful (23). Other factors that can contribute to message acceptance are a physician's concern, interest, friendliness or empathy toward the patient and the alliance that may form once trust is established (24). Thus, through the use of communication theory, a provider can influence and create positive behavioral change that might significantly improve patient adherence to daily medications and medical appointments (25). Before initiating ART, providers should take the time to discuss with the patient the advantages and disadvantages, risks and benefits of each medication protocol (26). An example would be when a patient might express concern about the possible side effects of a medication or treatment regimen. By presenting reliable treatment options and individualized treatment plans to patients and discussing options with them, they can be involved in the decision-making process. This is key and a cornerstone to the collaborative development of a successful treatment strategy.
The Cognitive Theory
The cognitive model emphasizes the beliefs and perceptions of patients as motivating behavioral factors. It also assumes health-related behavior is determined by an understanding of health benefits and the threats perceived in health behavior choices made by the patient (19). The primary model dimension is the perceived severity and probability of the threat and the perceived benefits and barriers of such behavior. Actions are based on the individual's subjective perception of the advantages and disadvantages, and are not necessarily based on rational objective computations (19). There are different cognitive concepts applied in adherence behavior studies. However, applying single cognition concepts in adherence behavior studies might not provide sufficient data, wihout considering other preexisting behavioral factors such as alcohol use disorders (27).
The Self-Regulation Model
The self-regulation theory is directed toward patient self-management, using educational interventions. It is determined by perceived social norms and/or group or social consequences (28). The theory maintains patients engage strategies that allow them to assume the role of active problem solvers. Thus, patient behavior is influenced by subjective emotions and experiences. These are based on perceptions of the goal and current status, the patient's plans to change his/her present state in order to achieve a goal, and the patient's appraisal to reach the target. When goals are altered or not achieved, a patient can change his/her perception and coping strategies (28). Coping among patients is based on cognitive considerations. The emotional and cognitive signals to cope are triggered by either external or internal stimuli (29). Media messages and symptoms are examples of external and internal stimuli.
2. Behavior-Specific Cognitions and Affect
This concept involves patient perception about the anticipated personal benefits of pursuing positive health outcomes that might result from a given health behavior (11). Thus, it entails situational influences, interpersonal influences, activity-related affect, perceived self-efficacy, perceived barriers to action, and perceived benefits of action.
Historically, most medication adherence studies describe patient forgetfulness as the greatest barrier to non-adherence (30 - 33). This is considered a non-intentional factor. Forgetfulness can be challenged and even improved as providers implement various reminder strategies such as cellular phone messages, alarms, emails, telephone reminders, and direct mail letters (17). Engaging the assistance of HIV patient caregivers establishes another route to removing non-adherence as a barrier to a medical regimen (34). Family-based or couples' interventions provide motivation and support for patients to adhere to their medication (35). Soliciting help from the HIV patient's family members and establishing trust via communication between the patient and the provider are vital components in assisting a patient toward self-efficacy and treatment adherence (36).
Providers monitor and evaluate patient adherence by using support, rewards, calendars, and diaries, as well as by providing concise and consistent feedback (37). Financial incentives were reported to improve adherence behavior to HIV management in the short-term and while the incentives were in place (38,39). However, only a few limited controlled studies have been reported to date (38).
Most research confirms that telephone prompts and mail reminders are beneficial in reducing patient non-adherence to scheduled medical appointments (40 - 42). One of the suggested intervention models that can be implemented easily by healthcare providers is a personal telephone call or a short reminder message sent a few days before a scheduled medical appointment. This kind of direct, personal communication reminds the patient of the importance of the pending medical appointment (17). Computerized reminders also are highly cost-effective and can motivate higher levels of adherence among HIV patients. As noted, adherence behavioral interventions are essential to improving adherence to scheduled medical appointments and daily medication, as medical providers seek to improve the health status of this highly vulnerable population.
The Behavioral Perspective Theory to Explain Adherence
Interventions based on incentives are essential to improving the HIV patient's adherence levels. Behavioral-adherent interventions are explained by using the behavioral theory. The model states the behavior of humans is largely based on cues or stimuli; these prompt specific responses that are essential in reinforcing behavior (19). Incentives can act as cues, reminders, and rewards for adherent behavior. The major principle of the behavior model is that behavior is learned by forming and/or gradually shaping behavior patterns. For a desired behavior to remain consistent, it must be reinforced through automation and frequent repetition. Reminders are, therefore, essential in improving adherence to scheduled medical appointments and daily medication. Due to advances in technology, reminders are the most inexpensive and direct intervention option available to HIV patients. By using electronic technology, these messages may be sent frequently by the provider, at little or no cost (43).
3. Behavioral Outcomes
The third HPM concept involves identification and intention of a planned strategy to implement a health behavior. It also can involve alternative behaviors that patients are not able to control because of environmental contingencies (12). Behavioral outcome interventions can be implemented by providers using technical strategies such as unit-dose and/or blister-packaging for medication, as compared to bottles and envelopes (13). With this model, the adherence strategies are aimed at reducing the number of drug types in the regimen or doses per day through the use of fixed-dose combination pills or extended release formulations. Fixed dose combination pills involve the formulation of two or more drugs in proportions that are set and/or blister packaged medicinal products in fixed dosage combinations. Additional adherence improvement aids include printed medication schedules and calendars that specify the time of day for daily medications and specific packaging such as pill boxes that indicate dosage frequencies (44).
The average rate of adherence is higher for a single daily dose compared to patients taking multiple daily doses (14). Therefore, treatment team members should consider dosing frequency when developing medication regimens and attempt to limit the number of daily doses required. Another strategy is the use of electronic medication container caps for elderly HIV patients who may have difficulty opening regular bottles (44). These electronic vial caps serve as a reminder system by beeping whenever a dose should be administered. The patient is rewarded with an accurate record of when medication(s) was (were) last dispensed. Therefore, the development and implementation of reliable medication-product modifications should be a priority in improving patient adherence.
Another important component of adherence involves follow-up appointments with the provider and the healthcare team. Wait times are an important factor and influence patient adherence to medical appointments. The longer a patient has to wait to schedule a visit to be seen by the provider, the lower the rate of adherence among the HIV-patient population (45).
There is robust and consistent evidence that indicates simplifying scheduled medical appointments and dosage regimens improves adherence by reducing the frequency of daily dosages (44). This can result in decreased health care costs and better health outcomes for HIV patients. As stated previously, a strong level of respect and professionalism must be developed between the healthcare provider and the patient in order to create this environment. Different therapeutic options and the manner in which they can be adhered to must be considered and implemented jointly by patients and providers. Acknowledgement of the crucial role each plays in the plan is critical to the development of trusting and respectful relationships between healthcare providers and patients.
The Biomedical Theory to Explain Adherence
The biomedical perspective theory assumes patients to be passive recipients of instructions and recommendations provided by treatment team members. It also discusses alternative behaviors patients are not able to control, based on environmental and technical contingencies. Thus, it envisions the identification of a planned best-managed strategy to implement health behavior(s). A disease such as HIV involves biomedical causes, and the predominant focus of treatment is restoration of health. Adopting the current advancement of a newer drug regimen is preferred (19). Technical adherence strategies simplifythe regimen by simplifing packaging and improving dosage adherence among HIV patients. Such interventions are part of a biomedical model in which providers seek solutions for HIV patients. The biomedical model, therefore, assists in motivating the development of technological advances in enhancing scheduled medical appointments and daily medication routines (19,20). In summation, simplification of treatment options is interpreted as a logical and practical solution.
Summary
In summary, no single adherence approach can resolve the status of commitment to patient adherence levels. Factors impacting adherence levels, such as the therapeutic relationship between treatment team members and the patient, should be addressed in an ongoing and/or proactive way (13). Adherence success is based on tailoring interventions to a patient's unique characteristics, readiness to engage in care, and the outcome expected from the treatment.
Collaboration between treatment team members and patients is still the foundational core of success in improving adherence behaviors. Negotiation, collaboration, engagement, and participation all enhance opportunities for an ideal therapeutic approach that will assist HIV patients as they develop the skills needed to maintain their adherence equation. Such partnerships influence patient adherence at all levels, foster patient satisfaction, and create positive healthcare outcomes. Thus, all of these critical adherence elements can be linked to retention and improved health outcomes in the care of HIV-infected patients.
Conventional interventions used to schedule medical appointments and reminders of daily medications, based on technical solutions, do not adequately explain the human situational thought processes. There is a need to present and utilize the components provided by the HPM before implementing such intervention(s). Adherence interventions such as reminders and incentives that stem from behavioral models are essential for non-adherent HIV patients who do not abide by their scheduled medical appointments and daily medications on a routine basis. It is unclear if educational, behavioral, biomedical and self-regulation models are more or less reliable in improving the level of adherence among HIV patients. Concentrated efforts to improve adherence can lead to a win-win solution in which healthcare providers, patients, and the community at large can all benefit. In order to effectively contribute to and validate the HPM, there is a need to promote and pursue further multidisciplinary, collaborative research that delves into the underlying issues of adherence as a cohesive team effort focused on improving healthcare for all HIV patients.
Conclusion
The paper contributes to advancement in the field by introducing the Health Promotion Model and describing its applicability to patient adherence behavior. The issue of adherence behavior in the HIV-infected population not only aligns with current research trends in United States (46), it also is the main research priority listed by the World Health Organization (9). Regardless of the types of HIV behavioral-related research topics, the HPM could still be appropriate as a foundation framework for interventions to address adherence. The challenge facing HIV patients has no simple solution in the area of behavioral change or adherence. The HPM can shed light on the processes underlying behavioral change. The theoretical model is essential for developing and implementing successful adherence interventions. More analysis is required to explore theory-based interventions in healthcare practices that are operative and developed based on a clear and relevant theoretical foundation. Finally, documentation shows that cohesive and dedicated teams of nurses spend the greatest amount of time with patients (10). To overcome adherence barriers and issues facing HIV patients with respect to daily medications and medical appointments , medical healthcare providers should be poised to assume a proactive role in promoting positive health habits over the long term through the Health Promotion Model.
References
1. Centers for Disease Control and Prevention. Primary care and public health initiative: Medication adherence. Centers for Disease Control and Prevention; 2013.
2. Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet (London, England). 2010;376(9738):367-87.
3. Mugavero MJ, Norton WE, Saag MS. Health care system and policy factors influencing engagement in HIV medical care: Piecing together the fragments of a fractured health care delivery system. Clinical Infectious Diseases. 2011;52(suppl 2):S238-S46.
4. Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. The New England Journal of Medicine. 2011;365(6):493-505.
5. Mills EJ, Nachega JB, Bangsberg DR, Singh S, Rachlis B, Wu P, et al. Adherence to HAART: A systematic review of developed and developing nation patient-reported barriers and facilitators. PLOS Medicine. 2006;3(11):e438.
6. Barnighausen T, Tanser F, Dabis F, Newell ML. Interventions to improve the performance of HIV health systems for treatment-as-prevention in sub-Saharan Africa: The experimental evidence. Current Opinion in HIV and AIDS. 2012;7(2):140-50.
7. Global Health Observatory (GHO) data [Internet]. 2015 [cited September 11, 2016]. Available from: http://www.who.int/gho/hiv/epidemic status/deaths/en/.
8. Martin LR, Williams SL, Haskard KB, DiMatteo MR. The challenge of patient adherence. Therapeutics and Clinical Risk Management. 2005;1(3):189-99.
9. World Health Organization. Priority interventions : HIV/AIDS prevention, treatment and care in the health sector: World Health Organization, HIV/AIDS Department; 2010. Report No.: 9789241596961 9241596961.
10. DeLucia PR, Ott TE, Palmieri PA. Performance in Nursing. Reviews of Human Factors and Ergonomics. 2009;5(1):1-40.
11. Pender NJ, Pender AR. Health promotion in nursing practice. Stamford, Conn.: Appleton & Lange; 1996.
12. McEwen M, Wills EM. Theoretical basis for nursing. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2011.
13. Thompson MA, Mugavero MJ, Amico KR, Cargill VA, Chang LW, Gross R, et al. Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: evidence-based recommendations from an International Association of Physicians in AIDS Care panel. Ann Intern Med. 2012;156(11):817-33.
14. Ryscavage P, Anderson EJ, Sutton SH, Reddy S, Taiwo B. Clinical outcomes of adolescents and young adults in adult HIV care. Journal of Acquired Immune Deficiency Syndromes (1999). 2011;58(2):193-7.
15. Parry MF, Stewart J, Wright P, McLeod GX. Collaborative management of HIV infection in the community: An effort to improve the quality of HIV care. AIDS Care. 2004;16(6):690-9.
16. Koenig SP, Bernard D, Dévieux JG, Atwood S, McNairy ML, Severe P, et al. Trends in CD4 Count Testing, Retention in Pre-ART Care, and ART Initiation Rates over the First Decade of Expansion of HIV Services in Haiti. PLOS ONE. 2016;11(2):e0146903.
17. Berg KM, Litwin A, Li X, Heo M, Arnsten JH. Directly observed antiretroviral therapy improves adherence and viral load in drug users attending methadone maintenance clinics: A randomized controlled trial. Drug and Alcohol Dependence. 2011;113(2-3):192-9.
18. Haukoos JS, Witt MD, Coil CJ, Lewis RJ. The effect of financial incentives on adherence with outpatient human immunodeficiency virus testing referrals from the emergency department. Academic Emergency Medicine. 2005;12(7):617-21.
19. Munro S, Lewin S, Swart T, Volmink J. A review of health behaviour theories: How useful are these for developing interventions to promote long-term medication adherence for TB and HIV/AIDS? BMC Public Health. 2007;7:104.
20. Armitage CJ, Conner M. Social cognition models and health behaviour: A structured review. Psychology & Health. 2000;15(2):173-89.
21. Osterberg L, Blaschke T. Adherence to medication. The New England Journal of Medicine. 2005;353(5):487-97.
22. Paasche-Orlow MK, Cheng DM, Palepu A, Meli S, Faber V, Samet JH. Health literacy, antiretroviral adherence, and HIV-RNA suppression: A longitudinal perspective. Journal of General Internal Medicine. 2006;21(8):835-40.
23. Merrill J, Kukafka R, Bakken S, Ferat R, Agopian E, Messeri P. Tailored health communication: Crafting the patient message for HIV TIPS. AMIA Annual Symposium Proceedings. 2003;2003:932-.
24. Sluijs EM, Knibbe JJ. Patient compliance with exercise: Different theoretical approaches to short-term and long-term compliance. Patient Education and Counseling. 1991;17(3):191-204.
25. Loeliger KB, Niccolai LM, Mtungwa LN, Moll A, Shenoi SV. "I have to push him with a wheelbarrow to the clinic.": Community health workers' roles, needs, and strategies to improve HIV care in rural South Africa. AIDS Patient Care STDS. 2016;30(8):385-94.
26. World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: Recommendations for a public health approach. World Health Organization; 2013. Report No.: 9789241505727 9241505729.
27. Parsons JT, Rosof E, Mustanski B. Medication adherence mediates the relationship between adherence self-efficacy and biological assessments of HIV health among those with alcohol use disorders. AIDS and Behavior. 2008;12(1):95-103.
28. Leventhal H, Lambert JF, Diefenbach M, Leventhal EA. From compliance to social-self-regulation: Models of the compliance process. Treatment compliance and the therapeutic alliance. 1997:17-33.
29. Delmas P, Delpierre C, Cote J, Lauwers-Cances V, Delon S. Study of the promosud cohort. Predictors of adherence to treatment plans by French patients living with HIV. Perspective infirmiere : revue officielle de l'Ordre des infirmieres et infirmiers du Quebec. 2008;5(7):28-35.
30. Hansana V, Sanchaisuriya P, Durham J, Sychareun V, Chaleunvong K, Boonyaleepun S, et al. Adherence to antiretroviral therapy (ART) among people living with HIV (PLHIV): A cross-sectional survey to measure in Lao PDR. BMC Public Health. 2013;13:617.
31. Polis S, Zang L, Mainali B, Pons R, Pavendranathan G, Zekry A, et al. Factors associated with medication adherence in patients living with cirrhosis. Journal of Clinical Nursing. 2016;25(1-2):204-12.
32. Roberts KJ. Barriers to and facilitators of HIV-positive patients' adherence to antiretroviral treatment regimens. AIDS Patient Care STDS. 2000;14(3):155-68.
33. Kagee A, Nel A, Saal W. Factor structure of the Beck Depression Inventory-II among South Africans receiving antiretroviral therapy. AIDS Care. 2014;26(2):257-62.
34.Lyon ME, Trexler C, Akpan-Townsend C, Pao M, Selden K, Fletcher J, et al. A family group approach to increasing adherence to therapy in HIV-infected youths: Results of a pilot project. AIDS Patient Care STDS. 2003;17(6):299-308.
35. Robbins RN, Spector AY, Mellins CA, Remien RH. Optimizing ART adherence: Update for HIV treatment and prevention. Current HIV/AIDS Reports. 2014;11(4):423-33.
36. Rachlis B, Naanyu V, Wachira J, Genberg B, Koech B, Kamene R, et al. Identifying common barriers and facilitators to linkage and retention in chronic disease care in western Kenya. BMC Public Health. 2016;16:741.
37. Smith V, Devane D, Begley CM, Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Medical Research Methodology. 2011;11(1):1-6.
38. DeFulio A, Silverman K. The use of incentives to reinforce medication adherence. Preventive Medicine. 2012;55(Suppl): S86-S94.
39. Petry NM, Rash CJ, Byrne S, Ashraf S, White WB. Financial reinforcers for improving medication adherence: Findings from a meta-analysis. The American Journal of Medicine. 2012;125(9):888-96.
40. Mayer JE, Fontelo P. Meta-analysis on the effect of text message reminders for HIV-related compliance. AIDS Care. 2016:1-9.
41. van Andel E, Been SK, Rokx C, van der Ende ME. Risk factors in an HIV-infected population for refraining from specialist care. AIDS Care. 2016;28(10):1255-60.
42. Madhvani N, Longinetti E, Santacatterina M, Forsberg BC, El-Khatib Z. Correlates of mobile phone use in HIV care: Results from a cross-sectional study in South Africa. Preventive Medicine Reports. 2015;2:512-6.
43. Leventhal H, Cameron L. Behavioral theories and the problem of compliance. Patient Education and Counseling. 1987;10(2):117-38.
44. Raboud J, Li M, Walmsley S, Cooper C, Blitz S, Bayoumi AM, et al. Once daily dosing improves adherence to antiretroviral therapy. AIDS Behav. 2011;15(7):1397-409.
45. Nachega JB, Parienti JJ, Uthman OA, Gross R, Dowdy DW, Sax PE, et al. Lower pill burden and once-daily antiretroviral treatment regimens for HIV infection: A meta-analysis of randomized controlled trials. Clinical Infectious Diseases : an official publication of the Infectious Diseases Society of America. 2014;58(9):1297-307.
46. The Henry J. Kaiser Family Foundation. U.S federal funding for HIV/AIDS: Trends over time. The Henry J. Kaiser Family Foundation; 2016.